INTRODUCTIONThe follow-up of patients with head and neck spinocellular carcinoma initially treated with curative intent is aimed at the locoregional recurrence diagnosis, specially in early clinical stage, and the objective is a higher probability of salvage treatment indication. Upon the presence of locoregional recurrence clinical suspicion, the inquiry with histological confirmation of the disease presence, clinical staging and complimentary imaging exams are performed, when necessary, for evaluation of the lesion extension and resectability (1).
In the locoregional recurrence early diagnosis, the salvage surgery is unquestionably the first treatment choice. The exclusive radiotherapy or the chemoradiation therapy is reserved to irresectable lesions and/or for patients in poor clinical conditions (2,3).
The treatment morbidity and the unfavorable prognosis must be considered by the doctor before the indication of salvage treatment, specially in the extensive local recurrences and with surgical salvage indication. Therefore, the evaluation as for the indication of treatment in the recurrences must be individualized and, in some scenarios, the ideal treatment for the patient is the palliative, even in the potentially resectable lesions and/or absence of previous irradiation (4).
Thus, the oral and oropharyngeal tumors have in the isolated virtual metastasis a rare event of the disease manifestation, with indexes of 5% to 20% (5-7). Then, the locally advanced disease exclusive diagnosis, the low indexes of virtual metastasis may be used as arguments favorable to the most aggressive treatment, that is, large resections and reconstructions, with safe oncological resectability limits or even strict resectability margins.
The regional recurrence treatment presents with better results with the surgical salvage, specially in the absence of regional metastasis in the early presentation and that were not submitted to cervical emptying, and the neck salvage surgery success is reserved previously submitted to cervical emptying (8,9).
Therefore, the patient's initial post-treatment follow-up is crucial for the early diagnosis of locoregional recurrences and/or virtual metastasis, and the ideal is the return of the patient in short intervals in the first two years, when 76% of recurrences occur (10). We found an index of 74% of locoregional recurrences diagnosis, and the first 18 months is the main period in the recurrences incidence (11).
The primary second tumors developed mostly in the anatomic site of the initial tumor or in other sites in the head and neck, followed by the esophagus and lung (12). The objective of the follow-up after the third year and with the diseased controlled may be specially the detection of a second tumor, with regular and prolonged returns.
The objective of this study is to evaluate the efficacy of the follow-up in the locoregional recurrence early diagnosis, in the indication of salvage treatment and its evolution and the virtual metastases and second primary tumors diagnosis.
METHODWe carried out a retrospective study of longitudinal historic cut of 276 medical reports of patients with oral and oropharyngeal spinocellular carcinoma, in the period from January 2009 through December 2005, in the Head and Neck Surgery and Otorhinolaryngology Department of the Hospital Heliópolis - Hosphel, São Paulo. The eligibility criteria were surgical initial treatment with curative intent and absence of previous oncological treatment. 28 patients with virtual metastasis were excluded in the initial presentation, previous treatment and presence of synchronous and simultaneous tumors.
According to the clinical stage (CS), and AJC-UICC (2002), the patients were divided into 26 cases of CS I; 71 CS II; 83 CS III and 96 CS IV. According to the anatomic site, 198 cases were of mouth and 78 of oropharynx. In the mouth, tongue and mouth floor, they represented 63.9% of the cases and in the oropharynx, tonsil region 64.1%. of the cases.
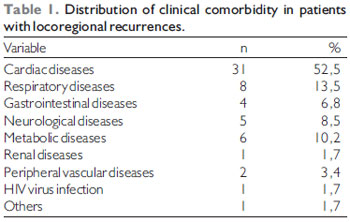
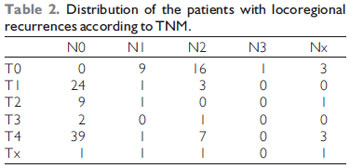
A hundred and twenty-seven patients evolved with locoregional recurrences, with average age of 54.6 years (ranging from 22 to 87 years old), and they were 106 (83.5%) men and 21 (16.5%) women. As for the previous history of smoking and alcohol, 22 patients didn't smoke and 51 didn't drink alcoholic beverages. No morbid history, 43 presented with a report of clinical comorbidity (Table 1). The distribution of size of the primary tumor (T) and the presence of cervical lymph nodes (N) in the 127 patients are described in Table 2.
All patients were submitted to the surgery as an initial treatment, and 231 cases were submitted to cervical emptying, out of which 150 unilateral emptying and 81 bilateral emptying. Only 19 cases were not submitted initially to cervical emptying for being neoplasms in initial CS and resections of tumors in the upper mouth floor. The postoperative complimentary radiotherapy was carried out in 121 patients with an average dose of 60.8Gy (20Gy to 70.4Gy). Seventeen cases had indication for postoperative radiotherapy and didn't undergo it because of complications of operative or clinical injury.
We considered to be locoregional recurrence the diagnosis made between the first 36 months of follow-up, and in the first 30 days of initial post-treatment, the patients didn't present with clinical evidence of disease. Only seven cases of local recurrence were diagnosed after 24 months. In all cases of salvage surgical treatment, there was histological confirmation of spinocellular carcinoma in the locoregional recurrence diagnosis.
The Institution's Ethics Committee in Research, where this study was carried out, approved of the research project of number 497. For evaluation of the quantitative variables the Chi-square methods and the Fisher's test were used. In the evaluation of differences of the patients' survival, we used the Log-Rank and Wilcoxon methods, and in the survival evaluation, we used the Kaplan-Meier's method. In the multivariate analysis the Cox models of Regression and Logistical Regression were used. The software programs used were Satistica, version 5.1 (Statsoft South America, Inc.), Tulsa, Oklahoma (EUA) and Epi Info, version 3.3.2TM, created by the CDC (Centers of Disease Control and Prevention).
RESULTSThe average follow-up was of 35.3 months, and in the patients with locoregional recurrence and submitted to the salvage treatment, the follow-up period deemed to be standard was that of 12 months. Fifteen (16.8%) patients has a follow-up shorter than 12 months, and from these six cases with a follow-up shorter than six months. There was no loss of follow-up.
Out of 127 cases of locoregional recurrences, 89 patients were submitted to salvage treatment, 76 to salvage surgery and the 13 remaining cases were forwarded for salvage chemoradiation therapy. Out of 76 cases submitted to salvage surgery, 23 underwent postoperative complimentary radiotherapy. The 38 remaining patients with locoregional recurrences were sent directly to the multidisciplinary palliative cares and five of whom because of refusal to surgical treatment and/or salvage chemoradiation therapy.
As for the CS in the locoregional recurrence, out of 127 patients, 25 were of CS I, 11 CS II, 16 CS III and 71 CS IV. In four patients it was not possible to evaluate the CS. As for the locoregional recurrence site, 37 were in oropharynx and 90 in the mouth. Fifty-four of these patients were submitted to postoperative radiotherapy, with an average dose of 59.8Gy (20 Gy to 70.4 Gy). In 23 cases there was indication for postoperative complimentary radiotherapy, which was not carried out because of operative injury complication in 16 cases. In the four remaining cases, there was no adherence of the patient.
The indication of exclusive radiotherapy salvage or chemoradiation therapy treatment was prescribed in the patients with absence of previous irradiation; presence of irresectable disease; Karnofsky performance status index higher than 70%; creatinine clearance higher than 30mL/m2 and refusal to salvage surgery (two cases). The radiotherapy was of teletherapy type, with linear accelerator device with average dose of 65.7Gy (40Gy to 72Gy) and chemotherapy with cisplatine (CDDP), dose of 30 mg/m2/week, in six cycles, beginning in the tenth fraction of radiotherapy. Eight patients underwent concomitant chemotherapy and the other were forwarded for exclusive irradiation. No patient needed interruption or pause of treatment for adverse effects.
The type of locoregional recurrence, according to the anatomic site and treatment determined in the 127 cases of recurrences, is schematized in Chart 1.
The initial post-treatment time interval and diagnosis median of the 127 locoregional recurrences is described in Graphic 1.
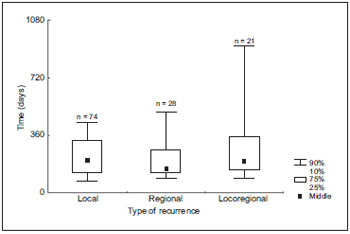
Graphic 1. Distribution of locoregional recurrences as for the interval between initial treatment and diagnosis.
As for the time interval between the locoregional recurrence diagnosis and the initial treatment of the 127 patients, in the period from one to six months of follow-up, 59 patients with locoregional recurrence were diagnosed; from six to 12 months, 43 patients in the period longer than 12 months, 25 patients. As for the results of the five-year disease-free survival in the 127 patients with locoregional recurrence, 13% in the locoregional recurrences were obtained up to six months of initial post-treatment; 40% in the locoregional recurrences between six months and 12 months; and 48% in the locoregional recurrences after 12 months of initial treatment (p = 0.00001).
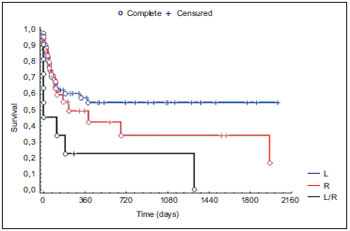
Upon association of the locoregional recurrence time with surgical salvage indication, 61% of salvage surgery were obtained; 51% between six to 12 months and 72% in the period longer than 12 months of follow-up. The salvage post-treatment disease-free survival (surgery with or without postoperative radiotherapy and chemoradiation therapy) of the 89 patients was statistically significant (p=0.0009) - Graphic 2.
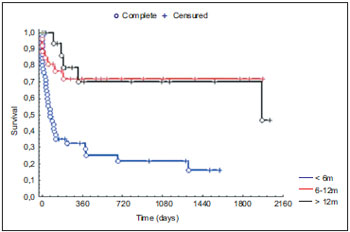
Graphic 2. Pos-salvage disease-free survival concerning the time interval between initial treatment and locoregional recurrence.
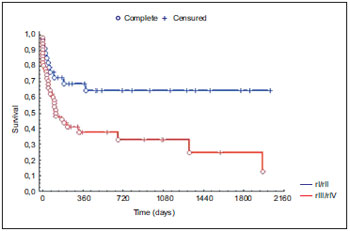
Out of the 89 cases treated in the locoregional recurrence, 53 cases of exclusive local recurrence treatment were observed, 25 in the exclusive regional and 11 in the locoregional. As for the accomplishment of surgical salvage, 62% and 74% were for exclusive local and regional recurrences, respectively, versus 31% of surgeries in the locoregional recurrences (p=0.004). Considering the type of recurrence treated in the salvage, the five-year disease-free survival was statistically significant (p=0.02) - Graphic 3.
Graphic 3. Post-salvage disease-free survival concerning the type of locoregional recurrence.
The CS in the locoregional recurrence diagnosis demonstrated a statistically significant difference in the five-year disease-free survival after salvage treatment of the 89 patients (p = 0.018) - Graphic 4.
Graphic 4. Post-salvage disease-free survival concerning the clinical stage in the locoregional recurrence.
The initial clinical stage and in the locoregional recurrence, as for the performance of salvage surgery, were statistically significant - Table 3.
The initial clinical stage and in the recurrence evaluated simultaneously in the 89 patients, as for the indication of salvage treatment, demonstrated a significant importance as for the five-year disease-free survival (p = 0.026) - Graphic 5.
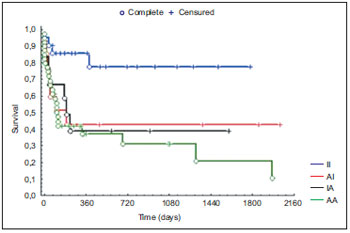
Graphic 5. Distribution of the initial clinical stage and in the locoregional recurrence concerning the disease-free survival after salvage treatment.
The five-year disease-free survival of the 89 patients submitted to salvage treatment was of 42.5% and the global survival of 47.5%. The disease-free survival according to the type of treatment, surgery, surgery and postoperative radiotherapy and chemoradiation therapy was statistically significant (p = 0.0017) - Graphic 6.
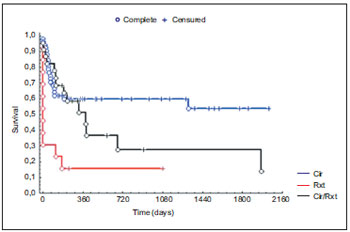
Graphic 6. Post-salvage disease-free survival distribution concerning the type of salvage treatment.
The five-year global survival of the 270 patients with follow-up was of 50.9%, whereas the global survival of the patients submitted to salvage treatment was of 45%.
Out of the 89 patients submitted to salvage treatment, 41 were alive and without disease, with an average follow-up of 25.7 months (considered as from the date of the first recurrence in all cases, including in the patients who developed a second locoregional recurrence). Thirty-eight patients died for locoregional and virtual disease; two died for other causes not related to the primary tumor treated and eight were alive and with disease in the follow-up period considered in the study.
In the follow-up period, 20 (7.2%) cases of virtual metastases were diagnosed, and they were multiple in three cases and with diagnosis time of 10.4 months (median). The higher frequency virtual metastases sites were lung (30.4%); skin (26.1%); bones (13%); armpits (7.3%); brain (7.3%); cranial base (7.3%); pleura (4.3%) and paravertebral musculature (4.3%).
As for the development of second primary tumor, 20 cases were diagnosed: 11 cases with primary tumor in the head and neck and with five-year disease-free survival of 70%. Amongst which, the diagnosis in six cases was in the first year of follow-up; five cases in the second year; three cases in the third year; four cases in the fourth year; one case in the fifth year and one case in the sixth year.
As for clinical comorbidity of the patients submitted to salvage treatment, two of whom died for other causes and with the disease locoregional and virtually control. The comorbidity was not responsible for retardation and/or interruption of the salvage chemoradiation therapy. Upon the last evaluation date, within the period considered in this study, the other patients submitted to salvage died as a result of the disease.
The clinical stage in the locoregional recurrence, the performance of previous radiotherapy and the recurrence anatomic site were the predictable factors for salvage treatment in the multivariate analysis - Table 4.
Logistical regression application; Const. ßO=10,17; n=122 locoregional recurrences, and the patients with clinical stage Tx or Nx in the locoregional recurrence were excluded.
In the multivariate analysis of the 89 patients submitted to salvage treatment, the type of salvage and the time interval between the initial treatment and the recurrence were significant factors in the disease-free survival - Table 5.
DISCUSSIONThe time interval between the diagnosis of the locoregional recurrence and the initial treatment is considered a prognostic factor for the indication of salvage treatment. The clinical distinction between the residual disease or development of a new tumor within the same cancerization field is impossible (13); therefore, the local recurrence definition is arbitrary. Thus, in the cases of recurrences up to six months of initial post-treatment, the clinical manifestation of disease may be residual disease (3,13). Faced with the early manifestation of initial post-treatment disease, the locoregional recurrences generally appear clinically as extensive lesions and many times with need for reconstruction. As for the cervical manifestation, they are usually related to the presence of voluminous lymph nodal disease and with capsular rupture. The resectability limits in the primary tumor may be narrow, a fact that leads us to a similar situation to that present in the recurrence, that is, the presence of active disease in the surgical bed (macroscopic or microscopic). In this study, 46.4% of the oral cavity and oropharynx spinocellular carcinoma locoregional recurrences were diagnosed in up to six months of follow-up, with five-year disease-free survival of 13%, which allows to suppose persistent or residual disease, considering the results found in the literature, ranging from zero to 26.7% of five-year global survival (3,14).
In the other hand, the recurrences considered to be delayed, after 12 months of initial treatment, usually present with better results in the disease control. Stell (1991) (15) demonstrated that the time interval of locoregional recurrence diagnosis and the initial treatment was statistically significant in the univariate and multivariate analysis. In the univariate analysis, it presented 20% less control of the disease in five years in the late recurrences. Our results are similar, with 19.7% of the locoregional recurrences diagnoses after 12 months of follow-up, with five-year disease-free survival of 48% (p = 0.00001). Goodwin (4), in turn, is the only author to report, in a metanalysis study of 1633 patients with various sites head and neck spinocellular carcinoma, that the recurrence time didn't obtain statistical importance in the control of the locoregional recurrence after the surgical salvage.
Poor results in the salvage surgeries in the locoregional recurrences diagnosed until six months after the initial treatment and promising results in the locoregional control in the late locoregional recurrences are demonstrated in several publications in the literature (2,3,16). The results of this study present with higher five-year disease-free survival indexes as for the salvage surgical treatment.
Thus, we may understand that the early locoregional recurrence (up to six months) would be bound to a disease in the advanced initial clinical stage, while the late locoregional recurrence (after 12 months) would be associated to the initial clinical stage disease. However, there are cases in the literature that don't shoe association of the initial clinical stage of the patient with the time of locoregional recurrence (4). But we had indication of salvage treatment with curative intent in 74.6% of the early locoregional recurrences, and 52.4% were of advanced clinical stage (III and IV) upon the patient's admission and only 22% were or early clinical stage (I and II) upon admission and with statistically significant findings in the relation of the salvage surgery with the initial clinical stage. Since the disease is clinically diagnosed at the presence of tumor in the locoregional exam, the local recurrence definition becomes difficult and arbitrary, because its manifestation may be residual or persistent disease in the primary tumor bed or, eve, a new tumor in the same site as initially treated.
Therefore, we are faced with paradigmatic prognostic factors, once a large part of the salvage treatment results, specially in this study, the salvage surgery, is poor in the presence of locoregional recurrence diagnosed early. Then, the salvage surgery diagnosed in the first six months of follow-up is not the ideal treatment for all patients with locoregional recurrence of advanced clinical stage (III and IV), even with resectable disease and patient with performance status index higher than 70%. Perhaps the tumor biological behavior is distinct in the initial presentation and in the locoregional recurrence, and translates into tumor genotype as a "new" disease, with a phenotype of presentation equal to the locoregional exam.
Only 10.2% of the patients underwent exclusive radiotherapy or salvage chemoradiation therapy, while in the literature the salvage irradiation indexes ranged from 8.6% to 28.9% (9,17-21). However, we obtained surprising and promising results in the one-year disease-free survival (17.6%), since 69.2% of the cases were of advanced clinical stage (III and IV) in the locoregional recurrence and also comparing them to results from zero to six or seven months of control of the disease. Schwatrz et al (3) were the only authors who demonstrated 12.6% of disease-free survival, similar to our finding.
Boysen et al (22) described similar results to those of this study, in which the development of second primary tumor is constant, as from the third year of follow-up and there is no decrease of its incidence in time. We consider our follow-up to be suitable in the diagnosis of second primary tumor, based on the patient's symptoms and signals and annual performance of simple radiography of the thorax and high digestive endoscopy (in the follow-up of oropharyngeal tumors), with diagnosis index of 7.4% in the period comprised in this study, since the performance of routine pan-endoscopy and computerized tomography may detect a malignant asymptomatic tumor of esophagus or lung. However, the cost-benefit ratio and the low control of the disease in these sites may lead to the questioning of the validity of such routine exams in the follow-up of the head and neck spinocellular carcinoma (12). A criticism may be the low index of virtual metastases diagnosis in this study within the period comprised, since the disease detection is basically made with the patient's reports and signal upon physical exam. It's worth remarking that 61% of the locoregional recurrences and virtual metastases of head and neck spinocellular carcinoma were diagnosed through the patients symptoms reported to the doctor and evidence of lesion in the exam, while only 39% were detected through exams, without evidence of the disease in the medical consultation (23).
The five-year disease-free survival of 70% of the patients treated for second head and neck spinocellular carcinoma confirms the findings in the literature, in which the disease control is similar to cases of locoregional recurrences diagnosed lately (4). Moreover, in some situations, the diagnosis of a second tumor in the same previous cancerization area or of lately diagnosed recurrence that remained quiescent for more than two years becomes difficult (2,11).
The incidence of isolated virtual metastasis in the literature works of oral and oropharyngeal spinocellular carcinoma follow-up presents with indexes of 5%, 7% and 20%, respectively; and we obtained isolated metastasis in 45% of the patients; except for one case, all were of advanced clinical stage in the patients admission (5-7). Such result resembles others, in which a higher index of isolated virtual metastasis was found and in the presence of advanced disease initially in the oral cavity and oropharynx (15). The virtual metastasis diagnosis for the cranial base may be questioned as a local or regional recurrence; however, the data obtained from the medical records and of difficult interpretation in the local and regional recurrence differential and metastasis for the cranial base were considered. Both cases were initially irradiated for advanced disease in the floor and basioglossus and presence of lymph nodes in level II affected by the disease. One of the cases was diagnosed with multiple virtual metastases.
Upon evaluation of the five-year disease-free survival and global survival of the patients in follow-up, we observed that the patients with oral cavity and oropharyngeal cancer had low indexes of death for other causes after the initial treatment. The main cause of death is represented by the locoregional and virtual recurrence. Upon evaluation of the five-year disease-free survival and global survival of the patients submitted to salvage treatment, we observed that the patients with oral and oropharyngeal spinocellular carcinoma had low indexes of death for other causes. The main cause of death is represented by the locoregional recurrence, which shows the event of the recurrence diagnosis is the main prognostic factor of the disease when associated to the variable comorbidity and neoplasm.
Therefore, the guidelines of hospital service follow-up of our patients proved to be suitable in the diagnosis of locoregional recurrence, with emphasis on the early clinical stage disease, as well as the patient's critical and quick management. The service consultations are monthly in the first 18 months and begins to be bimonthly until the third year. As from then, quarterly until the five years and six-monthly after five years.
CONCLUSIONThe importance of follow-up in the patients with oral cavity and oropharynx spinocellular carcinoma is a basic factor for the disease-free survival after the salvage treatment of locoregional recurrences, as well as the clinical stage in the recurrence, specially in an early clinical stage (I and II), for the indication of the type of salvage treatment.
BIBLIOGRAPHICAL REFERENCES1. Cooney TR, Poulsen MG. Is routine follow-up useful after combined-modality therapy for advanced head and neck cancer? Arch Otolaryngol Head Neck Surg. 1999, 125:379-82.
2. Amar A, Curioni OC, Franzi SA, Rapoport A. Recidivas locais após o tratamento cirúrgico do carcinoma epidermóide de cabeça e pescoço em estádio avançado. Rev Col Bras Cir. 2005, 32:60-3.
3. Schwartz GJ, Mehta RH, Wenig BL, Shaligram C, Portugal LG. Salvage treatment for recurrent squamous cell carcinoma of the oral cavity. Head Neck. 2000, 22(1):34-41.
4. Goodwin WJ. Salvage surgery for patients with recurrent squamous cell carcinoma of the upper aerodigestive tract: when do the ends justify the means? Laryngoscope. 2000, 110(3 Pt 2 Suppl 93):1-18.
5. León X, Quer M, Orús C, Venegas MP, López M. Distant metastases in head and neck câncer patients who achieved loco-regional control. Head Neck. 2000, 22(7):680-6.
6. Vikram B, Strong EW, Shah JP, Spiro R. Failure at distant sites following multimodality treatment for advanced head and neck cancer. Head Neck Surg. 1984, 6(3):730-3.
7. Lindberg RD. Sites of first failure in head and neck cancer. Cancer Treat Sympt. 1983, 2:21-31.
8. Amar A, Rapoport A. Recidivas regionais nos pacientes com carcinoma epidermóide das vias aerodigestivas superiores submetidos a esvaziamento cervical. Rer Col Bras Cir. 2003, 30(2):128-33.
9. Kowalski LP. Results of salvage treatment of the neck in patients with oral cancer. Arch Otolaryngol Head Neck Surg. 2002, 128:58-62.
10. Haas I, Hauser U, Ganzer U. The dilemma of follow-up in head and neck cancer patients. Eur Arch Otorhinolaryngol. 2001, 258:177-83.
11. Amar A, Franzi SA, Rapoport A. Evolution of patients with squamous cell carcinoma of upper aerodigestive tract. Sao Paulo Med J. 2003, 121(4):155-8.
12. Neel HB. Routine panendoscopy - is it necessary every time? Arch Otolaryngol. 1984, 110:531-2.
13. Slaughter DP, Southwick HW, Smejkal W. Field cancerization in oral stratified squamous epithelium. Cancer. 1953, 6:963-8.
14. Agra IMG, Kowalski LP. Fatores prognósticos em carcinoma epidermóide de boca e orofaringe submetidos a cirurgia de resgate. Radiol Bras. 2004, 37(6):424.
15. Stell PM. Time of recurrence of squamous cell carcinoma of the head and neck. Clin Otolaryngol. 1991, 13(4):277-81.
16. Leemans CR, Tiwari R, van der Wall I, Karim ABMF, Nauta JJP, Snow GB. The efficacy of comprehensive neck dissection with or without postoperative radiotherapy in nodal metastase of squamous cell carcinoma of the upper respiratory and digestive tract. Laryngoscope. 1990, 100:1194-8.
17. Pearlman NW. Treatment outcome in recurrent head and neck cancer. Arch Surg. 1979, 114:39-42.
18. Razack MS, Sako K, Patel JK. The role of initial modality in treatment of squamous cell carcinoma of the tongue. J Surg Oncol. 1982, 19:136-8.
19. Kokal WA, Neifeld JP, Eisert DR, Terz JJ, Lawrence Jr W. Management of locoregional recurrent oropharyngeal carcinoma. Am J Surg. 1983, 146:436-8.
20. Wong LY, Wei WI, Lam LK, Yuen APW. Salvage of recurrent head and neck squamous cell carcinoma after primary curative surgery. Head Neck. 2003, 25(11):953-9.
21. Eckardt A, Barth EL, Kokemueller H, Wegener G. Recurrent carcinoma of the head and neck: treatment strategies and survival analysis in a 20-year period. Oral Oncol. 2004, 40:427-32.
22. Boysen M, Lovdal O, Tausjö J, Winther F. The value of follow-up treated for squamous cell carcinoma of the head and neck. Eur J Cancer. 1992, 28(2):426-30.
23. Shaha A, Hoover E, Marti J, Krespi Y. Is routine triple endoscopy cost-effective in head and neck cancer? Am J Surg. 1988, 155(6):750-3.
1. In course for Post-Graduation Master's Degree in Health Sciences of Hospital Heliópolis - Hosphel, São Paulo. Surgeon of the Head and Neck Surgery and Otorhinolaryngology Department of Hospital Heliópolis - Hosphel, São Paulo.
2. Doctoral Degree in Medicine of the Post-Graduation Course in Oncology at the Medicine College of the University of São Paulo. Professor of the Post-Graduation Course in Health Sciences of Hospital Heliópolis - Hosphel, São Paulo.
3. Doctoral Degree in Medicine at the Post-Graduation Course in Otorhinolaryngology and Head and Neck Surgery of the Federal University of São Paulo - Escola Paulista de Medicina. Professor of the Post-Graduation Course in Health Sciences of Hospital Heliópolis - Hosphel, São Paulo.
4. Doctoral Degree in Medicine at the Post-Graduation Course in Otorhinolaryngology and Head and Neck Surgery of the Federal University of São Paulo - Escola Paulista de Medicina. Chief of the Head and Neck Surgery Service of Hospital Heliópolis - Hosphel, São Paulo.
5. Free Professor at the Medicine College of the University of São Paulo. Coordinator of the Post-Graduation Course in Health Sciences of Hospital Heliópolis - Hosphel, São Paulo.
6. Doctoral Degree in Medicine at the Post-Graduation Course in Otorhinolaryngology and Head and Neck Surgery of the Federal University of São Paulo - Escola Paulista de Medicina. Head Professor of Otorhinolaryngology and Head and Neck Surgery of the Metropolitan University of Santos.
Institution: Curso de Pós-Graduação em Ciências da Saúde do Hospital Heliópolis - Hosphel. São Paulo / SP - Brazil.
Mail address:
Rua Cônego Xavier, 276, 10º andar
São Paulo / SP - Brazil - Zip code: 04231-030
Article received on January 02, 2009.
Approved on February 25, 2009.