INTRODUCTIONA deficiency interferes with the perception of hearing and speech recognition for the child, causing a delay in the development of listening skills (detection, discrimination, recognition, understanding and attention). Thus, there are problems of understanding, communication and learning, reflected in low academic achievement and social isolation (1).
The prevalence of hearing loss in the general population, taking into account the losses mild bilateral or unilateral losses may exceed 7.7% of the people, reaching even higher rates in developing countries (1). BÉRIA et al. In an epidemiological survey on 2427 people in Rio Grande do Sul, found a prevalence of some degree of hearing loss in 26.1% of the population, while 6.8% have hearing disability (2).
The benefits of hearing screening in school children have been well demonstrated, but the provision of hearing screening programs has been restricted to large centers, due to shortage of equipment and skilled professionals in most cities in developing countries (1). Thus, it appears necessary to examine the most appropriate methods for use in countries with limited resources, using a minimum investment in equipment and training and that could be taught to primary health care workers.
The use of equipment already available in schools and health facilities as the computer would be an alternative to the purchase of specialized equipment. The possibility of using the Internet to download the program and conduct the training of the executors of the tests become unnecessary transport of materials and people, facilitating the dissemination of screening and improves the quality of screening programs (3). Telemedicine has been proposed as an alternative to alleviate these problems by allowing better quality healthcare to underserved populations in rural towns and cities, despite the difficulties caused by lack of personal contact and kinetics (4). However, there are no reports in the literature of methods to assess hearing distance that does not use a specific device in the remote point, as an audiometer, OAE equipment or auditory brainstem response, nor without the need for a specialized professional to operate the equipment so in person or remotely. This study aims to: (a) develop a screening method for remote identification of individuals with hearing loss requiring further investigation, (b) test its sensitivity, specificity and predictive values, (c) Compare it with audiometry screening.
METHODTeleaudiometry
The Teleaudiometry simulated on a computer, tools and patterns of an auditory screening carried out automatically by the software. The software can be installed on any computer with Windows XP® operating system and promotes the emission of pure tones of 1000, 2000 and 4000 Hz in each ear separately. With the aid of a noise analyzer, you can adjust the intensity of the stimulus delivered from an earphone (TDH 39). The algorithm implementation and testing of software is similar to that recommended by ASHA (1997) for an auditory screening (5). Following this standard, the software defines as negative screening cases in which the individual responds to at least two of three sounds to 20 dB at all frequencies tested (1000, 2000 and 4000 Hz) in each ear. If these criteria are not met, the program classifies the case as positive screening.
During the exam, the software detects any mouse click or spacebar held in a period of up to four seconds after emission of each tone, defining identification as an audible sound. The sounds are emitted at intervals of random duration between three and eight seconds, so that the individual provide their appearance.
After the testing software can send the results and data of individuals tested for a central database on the Internet. This facilitates the control and statistical data analysis and management of cases that need referral, with medical evaluation and / or speech therapy.
Casuistry
This study was approved by the Ethics Committee and Analysis of Research Projects, Faculty of Medicine, University of São Paulo as 713/05.
We included individuals aged between 17 and 50 years randomly selected from among patients and caregivers of Clinical Otorhinolaryngology, Hospital of the Faculty of Medicine, University of São Paulo (FMUSP). Were considered exclusion criteria:
a) Individuals with a history or signs of neuro-psychomotor.
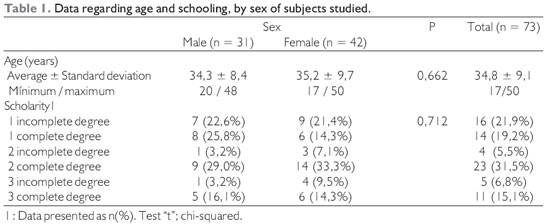
Thus, from September 2006 to March 2007 were included 73 individuals, 42 (57.5%) were female and 31 (42.5%) males. Data regarding age and schooling are presented in Table 1.
There was no statistically significant difference between the sexes regarding age and schooling.
All patients signed a consent form after being informed about the objectives and nature of the experimental study.
Equipment used in testing
Teleaudiometry program was installed on a laptop Brand HP ® Pavilion dv4000 with Intel® Centrino 2.0 GHz, 1024MB memory, 128 MB video memory, 100 GB HD, Sound Card SoundMAX Integrated Digital Audio® , operating system Microsoft® Windows® XP Home Edition and Professional headset TDH 39 with adapter connector P10 to P2 mono stereo. The computer was calibrated after determining the volume of the sound card and audio devices, using a noise analyzer (Bruel & Kjær model 2250) with artificial ear & Bruel and Kjær 4152 filter 1 / 1 and 1 / 3 of eighth (Bruel & Kjær model 1625) and microphone (Bruel & Kjær model 4144).
For screening audiometry (AV) was used an audiometer Beta Beta Medical ® model 6000 with TDH 39, and pure tone audiometry (PTA) audiometer Madsen Electronics ® Midimate model 622, with TDH 39, both calibrated two weeks before the start of testing in accordance with the standards of ANSI-1999 (6).
The ambient noise level during the screening tests was controlled with the aid of analyzer noise by observing the standards of ANSI-1999 (6).
Achievement tests
Selected subjects answered a questionnaire performed by the researcher with identifying data register and otological complaints. Then, patients underwent a bilateral otoscopy.
After answering the questionnaire, people were subjected to tests of auditory screening (AV), Teleaudiometry (TA) and pure tone audiometry (PTA) in random order and made the same day. During testing of AT and AV were measured noise environments, through the weighted equivalent sound level (LAeq) and maximum sound level (LAMAX), and time.
Prior to the completion of each exam, the individual received guidance on implementing it. The executors of the examinations of ATP and AV speech therapists were accredited by the Federal Council of Speech Therapy. In the case of ATP and AV, there was direct participation of the audiologist in achieving, measuring and interpreting results. Already in the TA, the role of the advisor was limited to orient the individual in the test, making the detection of responses and interpretation of results under the responsibility of the software. The executors of each test were unaware of the results of others.
The protocol for implementation of AV and TA was based on the standard of ASHA (1997) for hearing screening, or test with three tones at frequencies of 1000, 2000 and 4000 Hz at 20 dB (5). The tones were delivered in pulsed form, with three pulses of 300 ms. First, we tested the left and then right. The pure tone audiometry to pure tones in sound enclosure was performed according to standards of the Manual of Guidance of the Board of Speech (7). Were adopted as criteria for hearing loss in the pattern of ATP, the criteria for Davis & Silverman (8), which are based on the average of three frequencies (500, 1000 and 2000 Hz) above 20 dB HL in the better or worse ear .
After completion of the three methods, the tested individual was questioned in relation to the difficulty in implementing the TA and AV, sending a note from one to five (1. Very easy, 2. Easy, 3. Regular 4. Difficult; 5 . very difficult).
Statistical analysis
Data were stored and analyzed using SPSS for Windows (SPSS Inc. - Chicago, II) version 13.0.
Were considered statistically significant when P values were less than 0.05.
The differences between genders with regard to age and education were analyzed, respectively, by testing t-test and chi-square. To evaluate the accuracy of screening tests for hearing loss diagnosis was done through the calculation of sensitivity, specificity, positive predictive value and negative predictive value, using as gold standard pure tone audiometry in acoustic booth. For comparison of the ambient noise during testing of AV and AT tests were paired t. The comparison between the degrees of difficulty encountered during the screening tests were performed using chi-square.
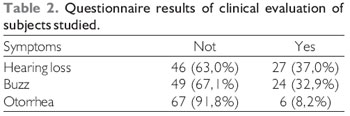
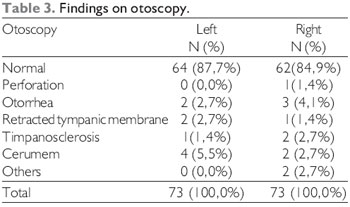
RESULTSThe 73 individuals included in the study underwent a questionnaire ear complaints (Table 2) and otoscopy (Table 3).
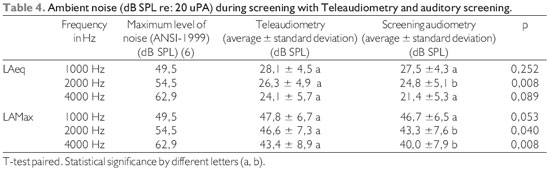
The ambient noise levels during the testing of AV and AT, shown in Table 4, were below the limits established by ANSI-1999 (6). During the performance of two screening methods (AV and TA), noise levels were shown to be below the maximum allowed at all frequencies, but there was a lower level of LAeq at 2000 Hz (p <0.05) during AV and lower levels of LaMax in 2000 and 4000 Hz (p <0.05) also during the AV.
The time of the Teleaudiometry ranged from 113 s to 193 s with a mean of 125 ± 11 s and the VA ranged from 40 s to 129 s with a mean of 65 ± 18 s.
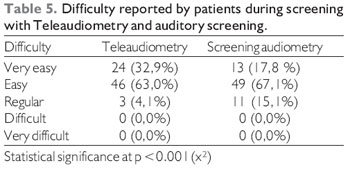
Individuals who underwent the screening tests indicated a low degree of difficulty when performing screening tests, as shown in Table 5.
Data regarding the accuracy of screening tests for diagnosis of hearing loss, using as the gold standard pure tone audiometry, are shown in Table 6.
DISCUSSIONIt is estimated 7.7% of the population have some degree of hearing loss, observing an increase in prevalence with increasing age and more frequently in developing countries (1). The sample with 37% of people with complaints of hearing loss, tinnitus in 32.9% and 8.9% with otorrhea due to the fact of selection have been performed on otolaryngological clinic of a referral hospital (Table 2).
The normal otoscopy in approximately 85% (87.7% and 84.9% left ear right ear - Table 3) of individuals is consistent with findings in other studies that show a low sensitivity of otoscopy in detecting people with hearing loss, because in most of them otoscopy is normal, and this method is dependent on the technical capacity of executor, has low reproducibility (9, 10).
The hearing screening is usually performed in an environment with no soundproofing, so that the noise environment can influence the test results. The ambient noise levels found in the study, presented in Table 4 remained below the recommended by ANSI (6) at all frequencies and decreased with increasing frequency evaluated, which is consistent with findings in the literature (11, 12).
The time of the Teleaudiometry proved reasonably rotating around 125 s, but it took about twice the time of AV (65 ± 18 s). According to the results obtained for every 60 individuals tested would need at least one more time to test if the Teleaudiometry was chosen instead of the auditory screening.
Individuals subjected to screening tests reported low degree of difficulty to perform them, as shown in Table 5, with a significantly lower upon Teleaudiometry (p <0.001). This may be due to greater concentration during Teleaudiometry, as the patient interacts directly with the computer and observe their responses on the screen.
The sensitivity of 86.7% found for the tests of auditory screening and Teleaudiometry reflects the similarity of the results of both methods. This result was expected since the protocol implementation and interpretation of the two methods are similar. The doubt on the efficiency of Teleaudiometry would be the possibility of the computer does not have sufficient stability to replicate the results satisfactorily or there is difficulty in performing the test. This doubt was cured by the similar performance to the test with audiometer and stability found during the calibration of the computer during the test, no adjustments are needed. The results in sensitivity are consistent with those found by other authors, ranging between 82 and 100% (13, 12, 14, 15). This variation in sensitivity of the method of screening audiometry is due, among other factors, the use of thresholds and different techniques for screening and to define hearing loss (12). The adoption of different criteria for hearing loss leads to different results on the test used as standard. Thus, studies that adopt criteria with higher thresholds tend to have higher sensitivity for the screening test (13). You can demonstrate this by observing the increased sensitivity of Teleaudiometry and auditory screening to 100% as a criterion in considering the presence of hearing loss threshold of the frequencies of 500, 1,000 and 2,000 Hz above 40 dB (mild hearing loss - DAVIS and SILVERMAN (8)).
Even without using the frequency of 500 kHz, there was not a departure from the results of the studies included in this frequency protocol (12, 13, 14, 15). Thus, it is prudent not to recommend the use of this frequency since the ambient noises tend to be more intense in low frequencies (16) and most of the places where these methods of hearing screening will be used in practice not provide equipment to measure noise and are admittedly noisy environments.
The specificity of Teleaudiometry (75.9%) was slightly higher than the audiometric screening (72.4%). This difference may be due to chance or to more easily found by individuals in achieving Teleaudiometry. The specificity of the auditory screening generally varies in the range between 65,9-99,0%, with most studies between 70.0 and 80.0% (1, 12, 13, 14, 15).
Compared to other techniques for sorting, teleaudiometry shows up as a good option, because it showed similar results for auditory screening, which according to a recent systematic review remains one of the methods the best results regarding sensitivity and specificity to the binomial (1). Audiometry screening has the disadvantage of needing equipment and skilled professionals, which prevents their use in most places outside major urban centers and makes this method economically disadvantageous, especially in developing countries like Brazil. In patients with limited understanding, probably the day of telaudiometria will be undermined, and in these cases, the presence of a qualified professional will facilitate the implementation of the test. In addition, an audiologist or otologist may recognize other communication disabilities and / or cognitive skills during the assessment. Thus, Teleaudiometry appears as a viable alternative for sites with a shortage of trained professionals in screening audiometry.
The Teleaudiometry had a higher sensitivity than that found in most studies using tympanometry (1, 17, 18).
In populations that are difficult to collaboration, as younger children or with some degree of neuro-psychomotor retardation, otoacoustic emissions, particularly transient, appear to have better results. However, our data suggest, in agreement with the literature findings, in the general population, the Teleaudiometry and auditory screening methods show themselves as superior, showing higher sensitivity and lower specificity (15, 19).
Other studies have sought methods of low-cost alternative to existing methods for screening hearing. The questionnaire to parents have proven methods such as low reproducibility, with great variation in the results of sensitivity and specificity, so that most authors agree that the questionnaires are flawed methods should only be used in the absence of more effective methods (1).
The method of video test, which was used in national campaigns for screening hearing in Brazil in 1999 and 2001, has the advantage of using equipment widely available in schools and health units, such as television and a video player, but fails reproducibility, lack of standardization and inefficiency in identifying unilateral loss (20). It was precisely these difficulties have stimulated the idealization of this study.
Other methods that use telemedicine for tests in places with scarce resources, such as remote computer equipment audiometric test enables individuals in remote locations with good results, but require sophisticated equipment (4, 22, 23 ). These systems are unworkable in practice in developing countries due to economic constraints.
You cannot raise a discussion on implementation of hearing screening programs, without questioning the viability of the economic point of view and availability of manpower and equipment. In countries with economic restrictions it becomes even more important. It's no good just to demonstrate the high accuracy of a method because it does not guarantee the applicability in practice. It is necessary to consider the most appropriate methods for use in countries with limited resources, using a minimum investment in equipment and training and that could be taught to primary health care workers (3). In this context, Teleaudiometry respect the parameters of good accuracy and simplicity of implementation and training facility of the applicators of the test. Moreover, the method uses equipment that is already partly available on the possible sites of use as schools and basic health units, requiring only an adaptation of the computer by purchasing a headset specific. The possibility of using the Internet to download the program and conduct the training of the executors of the tests makes it unnecessary to transport materials and people, facilitating the diffusion of this method in countries with continental dimensions like Brazil.
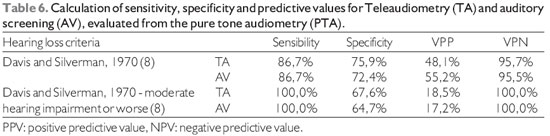
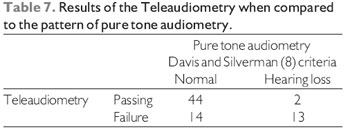
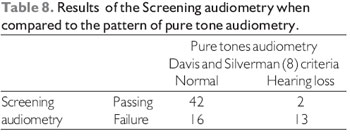
The Teleaudiometry proved to be a good option as a method of hearing screening, with accuracy close to the auditory screening. Compared to this method, the telaudiometria showed similar sensitivity (86.7%), higher specificity (75.9% vs. 72.4%) and negative predictive value (95.7% vs. 95.5%) and lower positive predictive (48.1% vs. 55.2%).
BIBLIOGRAPHICAL REFERENCES1. Bamford J, Fortnum H, Bristow K, Smith J, Vamvakas G, Davies L, et al. Current practice, accuracy, effectiveness and cost-effectiveness of the school entry hearing screen. Health Technol Assess. 2007, 11(32).
2. Béria JU, Raymann BCW, Gigante LP, Figueiredo ACL, Jotz G, Roithman R, Selaimen da Costa s, Garcez v, Scheres C, Smith A. Hearing impairment and socioeconomic factors: a population-based survey of an urban locality in southern Brazil. Rev Panam Salud Publica. 2007, 21(6):381-7.
3. Prescott CA, Omoding SS, Fermor J, Ogilvy D. An evaluation of the 'voice test' as a method for assessing hearing in children with particular reference to the situation in developing countries. Int J Pediatr Otorhinolaryngol. 1999, 51(3):165-70.
4. Givens GD, Elangovan S. Internet application to tele-audiology-"nothin but net". Am J Audiol. 2003, 12(2):59-65.
5. American Speech-Language-Hearing Association (1997). Guidelines for Audiologic Screening [Guidelines]. Retrieved September 12, 2008 from www.asha.org/policy.
6. American National Standards Institute (1969). Maximum permissible ambient noise levels for audiometric test rooms, ANSI 1999. New York: the Institute.
7. Conselhos de Fonoaudiologia (2007). Manual de orientação ao fonoaudiólogo que atua na área da Audiologia. Retrieved september 03, 2008 from www.fonoaudiologia.org.br.
8. Davis H, Silverman SR (1970). Hearing and Deafness. Holt: Rinehart and Winston.
9. Olusanya B. Early detection of hearing impairment in a developing country: what options? Audiology. 2001, 40(3):141-7.
10. New Zealand Health Technology Assessment. Screening programmes for the detection of otitis media with effusion and conductive hearing loss in pre-school and new entrant school children: a critical appraisal of the literature [structured abstract]. NZ Health Technol Assess. 1998, 3:61.
11. Hallett CP, Gibbs AC. The effect of ambient noise and other variables on pure tone threshold screening in a population of primary school entrants. Br J Audiol. 1983, 17(3):183-90.
12. FitzZaland RE, Zink GD. A comparative study of hearing screening procedures. Ear Hear. 1984, 5(4):205-10.
13. Orlando MS, Frank T. Audiometer and AudioScope hearing screening compared with threshold test in young children. J Pediatr. 1987, 110(2):261-3.
14. Holtby I, Forster DP, Kumar U. Audiometria de tons puros and impedance screening of school entrant children by nurses: evaluation in a practical setting. J Epidemiol Community Health. 1997, 51:711-15.
15. Sabo MP, Winston R, Macias JD. Comparison of pure tone and transient otoacoustic emissions screening in a grade school population. Am J Otolaryngol. 2000, 21(1): 88-91.
16. Lankford JE, Perrone DC, Thunder TD. Ambient noise levels in mobile audiometric testing facilities: compliance with industry standards. AAOHN J. 1999, 47(4):163-67.
17. Barlow J, Stewart-Brown S, Fletcher J. Systematic review of the school entry medical examination. [review]. Arch Dis Child. 1998, 78(4):301-11.
18. Roush J, Drake A, Sexton JE. Identification of middle ear dysfunction in young children: a comparison of tympanometric screening procedures. Ear Hear. 1992, 13(2): 63-9.
19. Nozza RJ, Sabo DL, Mandel EM. A role for otoacoustic emissions in screening for hearing impairment and middle ear disorders in schoolage children. Ear Hear. 1997, 18(3):227-39.
20. Mangabeira PL, Bento RF. A fonoaudiologia na campanha. Acta AWHO. 2000, 19(4):211-12.
21. American Speech-Language-Hearing Association (2001). Telepractices and ASHA: Report of the Telepractices Team. Retrieved September 12, 2008 from www.asha.org/policy.
22. Elangovan S. Telehearing and the Internet. Seminars in Hearing. 2005, 26(1):19-25.
23. Krumm M, Ribera J, Klich R. Providing basic hearing tests using remote computing technology. J Telemed Telecare. 2007, 13(8):406-10.
1. Doctor. Otolaryngologist.
2. Full Professor. Professor of Otorhinolaryngology, Faculty of Medicine, University of São Paulo.
Instituition: Faculdade de Medicina da Universidade de São Paulo. São Paulo / SP - Brazil. Mail Address: Victor Eulálio Sousa Campelo - Avenida José dos Santos e Silva, 1520 - Teresina / PI - Brazil - ZIP CODE: 64001-300 - Telefax: (+55 86) 3223-6983 - E-mail: vcampelo@yahoo.com.br. Floating: Fundação de Amparo à Pesquisa do Estado de São Paulo. Article received in February 23, 2010. Article approved in March 13, 2010.