 |
566 |
|
| Year: 2008 Vol. 12 Num. 4 - Out/Dez - (7º)
|
|
 |
| Section:
Original Article
|
|
|
|
|
| Quality of Life Questionnaire Application in Patients Before and After Vestibular Rehabilitation |
|
| Author(s): |
| Lucia Kazuko Nishino1, Lídio Granato2, Carlos Alberto Herrerias de Campos2
|
|
|
| Key words: |
| dizziness, vertigo, quality of life, rehabilitation |
|
|
 |
| Abstract: |
Introduction: Conventional vestibular tests are not efficient instruments to evaluate the level of commitment in the life quality of a patient with dizziness. The quality of life questionnaire specific for dizziness, the Dizziness Handicap Inventory, was translated and validated into Portuguese intending to get over this difficulty in quantifying the vertiginous patient symptoms. Objective: This study aims at comparing the Brazilian Dizziness Handicap Inventory results before and after personalized vestibular rehabilitation in patients diagnosed with chronic vertigo from benign paroxist positional vertigo and chronic vertigo from other causes. Method: Retrospective study of 30 medical records; all of which were submitted to the Brazilian Dizziness Handicap Inventory before and after the personalized vestibular rehabilitation treatment. Results: In the total scores average of vestibular pre-rehabilitation, the benign paroxist positional vertigo had a score of 47.93±24.46 and the chronic vertigo for other causes of 54.40±20.97. At discharge, the benign paroxist positional vertigo scores average was of 6.13±7.22 and in the chronic vertigo from other causes, the scores average was of 26.13±20.51. Conclusion: The commitment of the life quality of individuals with dizziness, both for chronic vertigo from other causes and benign paroxist positional vertigo, was very similar, confirming an important commitment. The vestibular rehabilitation effect for both cases was also efficient and the Dizziness Handicap Inventory was an efficient instrument to evaluate the vertiginous case evolution.
|
|
 |
INTRODUCTION
Dizziness is a symptom that reaches 10% of the worldwide population (1). It's appointed as the most common complaint in the world after 65 years of age (2). It may be associated with a single symptom, but many times it's also followed by other signs and symptoms, such as several kinds of auditory changes and neurovegetative disturbances (3).
One of the reasons that makes dizziness such a frequent symptom is its etiologic diversity that may include, in addition to a series of local (labyrinthic) causes, cardiovascular, neurological, orthopedic, hormonal, autoimmune, genetic, infectious, inflammatory, psychological and psychiatric factors. There's a large number of causes for dizziness, and they are described in around 30 otoneurologic clinical pictures, with different manifestations. Such variety may also be explained by the very labyrinth physiologic structure, both in the vestibular as in the auditory portions, which are very sensitive to changes of other parts of the body and frequently the etiological agent of the vestibular dysfunctions is represented by a virtual affection (4,5).
The benign paroxist positional vertigo (BPPV) is a chronic disease of recurrent clinical course; the maneuvers efficiency has been questioned, since BPPV presents with a high rate of spontaneous remission above 30% (6).
In spite of the otoneurological diagnosis advance, with computerized records and a major precision in these exams findings, the vestibular system tests are not particularly sensitive or specific to describe the possible psychological interference with the clinical picture and in the affection of the patient with dizziness (7).
Aiming at quantifying the dizziness interferences, both physically and functionally or emotionally in the vertiginous individual's everyday activities, Jacobson e Newman (8) prepared and validated a specific questionnaire, the Dizziness Handicap Inventory (DHI), in order to evaluate the self-perception of the incapacitating effects imposed by dizziness.
The DHI was translated from English into Portuguese and submitted to cultural adaptation, linguistic adaptation, review of grammatical and idiomatic equivalence and intra- and inter searchers reproducibility (9,10).
The effect of the vestibular system changes treatment, whether medication-related, surgical or for rehabilitation, may also be followed-up and measured by means of a life quality questionnaire (9).
Many studies show the importance of evaluating the life quality damages to help in the choice of treatment or even for a change in the therapy used. The objective of this work was to compare the Brazilian DHI results before and after Personalized Vestibular Rehabilitation (PVR) in patients with diagnosis of chronic benign paroxist positional vertigo and chronic vertigo for other reasons.
METHOD
30 records were selected of female sex patients who finished the treatment with Vestibular Rehabilitation in the Otorhinolaryngology Service in the Institution's Otoneurology Department, in the years 2004 and 2005, and 15 with the diagnosis of chronic vertigo for other causes (CVOC) and 15 with chronic vertigo (BPPV).
The inclusion criteria for both groups was the clinical history of dizziness with more than three months of evolution
All ethical principles were respected according to resolution 196/96 (MINISTRY of Health, 1996) on ethics in human beings research and the guidelines of the Research Ethics Committee - of the institution, by protocol no. 056/06.
The patients studied were not using any medication specifically for dizziness.
These 30 patients answered the everyday life questionnaire, the Brazilian DHI, composed by twenty-five questions (Annex 1), comprising seven questions evaluating the physical aspect, nine the emotional aspect and seven the functional aspect.
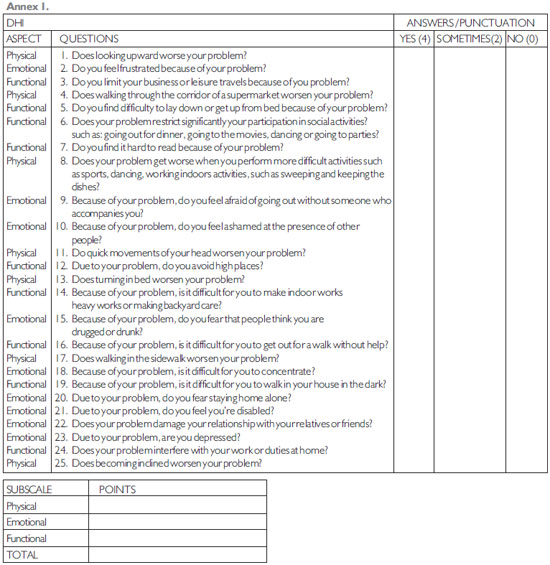
The patients were instructed to answer each question only with the following answers: "yes", "no" or "sometimes". For each "yes" answer 4 points were added, for each "no" 0 points and for each "sometimes" answer, 2 points were added. Therefore, the higher the score values were the higher were the "damages" in the life quality.
The questionnaire was applied before and after treatment.
The treatment carried out in these cases was the vestibular rehabilitation, whose type ranged, depending on complaints and the diagnosis of each patient. For patients with CVOC personalized exercises were used, according to the difficulties and facilities of each individual. For those with BPPV the Epley repositioning maneuver was used in all cases. All patients were instructed to weekly turn-arounds to verify the evolution of each case.
The statistical treatment used to evaluate the results was the Wilcoxon test for parallel samples. The significance level used was of p<0.05 (5%). When the statistics calculated presented statistically significant difference we used asterisk (*), for non-significant differences no marker was used, only the value of p.
RESULTS
The fifteen patients with CVOC were between 16 to 78 years old and the average±standard deviation were of 50.93±17.69 The fifteen patients with BPPV diagnosis were from 47 to 87 years of age with 58.40±10.07. In the statistical analysis by Wilcoxon's test no statistically significant difference was found (p=0.3941) between the two groups studied.
The two groups chronicity, measured per months, was of 30.20±20.98 for CVOC and of 9.07±6.74 for BPPV with statistically significant differences (p=0.0029*).
The reasons regarding the patients with CVOC were: 8 (53.33%) from metabolic source, 5 (33.33%) from vascular source, 1 (6.67%) from encephalic cranial traumatism and 1 6.67%) for sickle cell anemia.
All patients who answered the Brazilian DHI before the treatment presented with some damage in the life quality (Table 1 and 2).
The total scores average of both pre-treatment groups didn't prove to be very different; for CVOC it was of 54.4±20.97 and for BPPV of 47.93 ±24.46. When both groups were compared we found p=0.4548.
In the performance of the Vestibular Rehabilitation (VR) an average of 9.67±4.67 sessions was carried out for CVOC patients, while for BPPV an average of 3.73±3.26 sessions were necessary, with p= 0.0002*.
Upon VR's discharge all patients answered the Brazilian DHI again (Table 1 and 2).
The total scores average for CVOC was of 26.13±20.51 and for BPPV it was of 6.13±7.22.
A diminishing of the score values was observed when compared to the pre-treatment values. Both for CVOC (p=0.002*) and BPPV (p=0.0000*) the results were significant compared to the pre- and post-treatment.
Upon analysis of the post-treatment difference between CVOC and BPPV a significant difference is also observed between both groups, since the BPPV patients improved more than those with CVOC (p=0.0012*).
DISCUSSION
The quantification of the limiting effects a disease causes to the individual's life quality may bring important information, both to forward an adequate therapy and to change it, because it brings information on the symptoms evolution and these symptoms reflection in the physical, emotional and functional aspects (8).
The average age evaluated in both groups ranged from 50 to 60 years. According to some authors (8,12), dizziness is more prevalent in old-aged individuals who tend to present a more affected corporal balance, because aging commits the central nervous system abilities in the performance of the vestibular, visual and self-perceptive signs processing responsible for the corporal balance, as well as decreases the capacity for modification of the adaptation reflections. It also results in a progressive loss of ciliated cells of peripheral sensorial receivers, decrease of the number of fibers and of the vestibular nerve myelinization, degeneration of ganglion cells and terminations of the peripheral and central vestibular system. In the BPPV the incidence increases 38% at each decade of life and 9% of the geriatric population have this disease diagnosis (13).
As for the gender, only women were chosen, since in the female sex the dizziness prevalence is higher reaching the proportion of 2:1 (3).
The number of required sessions for discharge of our patients coincided with that of other authors (14,15), who also needed less sessions for the BPPV than for CVOC (15,16).
In the pre-treatment Brazilian DHI answers similar scores were observed between patients with CVOC and BPPV. For all aspects the patients had high scores, mainly the functional aspect, which has questions regarding the social activities. Such results were also found in other studies (8,17), in which many patients deliberately restrict their physical activities, travels and social meetings in order to diminish the risk of unpleasant symptoms (Tables 1 and 2).
In BPPV very similar scores were also observed both for the functional and physical aspects, because in the BPPV the appearing of symptoms is closely related to certain cephalic positions and movements, whose relevant questions are contained in the physical aspects of the Brazilian DHI (8).
In our work the high indexes for the emotional aspects were also observed in both groups. Patients with changes in the Vestibular System many times present with anxiety associated to panic attacks, fear of going out alone and feeling of depersonalization, and remark the relationship between the vestibular changes and the emotional aspects (8).
All BPPV patients who finished the treatment presented with a difference between the pre- and post-treatment scores higher than 18 points and mentioned a significant improvement of the symptoms. For the DHI authors, a difference of 18 points between pre and post-treatment would indicate a significant change which could be deemed to be a benefit (9). As for those with Chronic Vertigo, 3 patients could not achieve a difference of 18 points and in these cases the DHI results coincided with the information of patients who mentioned a partial improvement of the symptoms and even a worsening of the picture as in the case of patient number 5. Such patients (20%) who didn't benefit from PVR were forwarded to the otorhinolaryngology service for new therapeutic guidelines.
In the CVOC there are several factors that bay result in dizziness, as well as a wide diversity of clinical pictures. This many times makes the treatment exclusively by Vestibular Rehabilitation inefficient and other therapies more adequate for each case are necessary.
CONCLUSION
1. The Brazilian DHI scores in the pre-treatment, both for chronic vertigo for other causes, as well as for BPPV were very similar and confirmed important interferences in both groups' life quality.
2. The VR improved the life quality of both groups.
3. In the post-treatment, the patients with BPPV presented with a better life quality when compared to carriers of chronic vertigo for other causes.
BIBLIOGRAPHICAL REFERENCES
1. Ganança MM, Caovilla HH. A otoneurologia no limiar do terceiro milênio. In: Ganança MM. Vertigem tem cura? São Paulo: Lemos Editorial. 1998; 263-70.
2. Ganança FF, Ganança CF. Vertigem na Infância e na adolescência. In: Ganança MM. Vertigem tem cura?São Paulo: Lemos Editorial. 1998; 37-47.
3. Campos CAH. Principais quadros clínicos no adulto e no idoso In: Ganança MM. Vertigem tem cura?São Paulo: Lemos Editorial. 1998; 49-58.
4. Ganança FF, Perracini MR, Ganança CF. Reabilitação dos distúrbios do equilíbrio corporal. In: GanançaMM (coord).Vertigem: abordagens terapêuticas. Fascículo III. São Paulo: Lemos; 2002.
5. Silva MLG, Munhoz MSL, Ganança MM, Caovilla HH. Quadros clínicos otoneurológicos mais comuns. São Paulo: Editora Atheneu; 2000.
6. Escámez JAL et al. Evalución Del tratamiento Del vértigo posicional paroxístico benigno mediante el cuestionario DHI-S. Acta Otorrinolaringol.Esp. 2001, 52:660-6.
7. Ganança FF, Castro ASO, Branco FC, Natour J. Interferência da tontura na qualidade de vida de pacientes com síndrome vestibular periférica. Rev Bras Otorrinolaringol. [periódico na Internet]. 2004 Jan [citado 2007 Ago 06]; 70(1): 94-101. Disponível em: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0034-72992004000100016&lng=pt&nrm=iso. Jacobson GP, Newman CW. The development of the Dizziness Handicap Inventory. Arch Otolaryngol Head Neck Surg. 1990;116:424-7.
8. Castro ASO. Dizziness Handicap Inventory: adaptação para o português brasileiro, aplicação, reprodutibilidade e comparação com os resultados à vestibulometria [tese].São Paulo: Universidade Bandeirantes de São Paulo; 2003.
9. Ganança FF, Castro ASO, Natour J, Branco FCA. Dizziness Handicap Inventory: cross-cultural adaptation to Brazilian Portuguese, its application, reproducibility and comparison with the vestibular evaluation results. Arch for Senso Neuro Sci Prac [periódico online] 2003a [cited 2003 Apr10]; (Apr 10): [6 screens}. Available from: http: www.neurootology.org/search/?PHPSSESSID=(d599f3231e4f0283564be73236f&m=c&v=3
10. Gushiken P, Caovilla HH, Ganança MM. Avaliação otoneurológica em idosos com tontura. Acta Awho.2002, 21(1):[25 telas].
11. Dannenbaum E, Rappaport JM, Visitin M, Fun J, Watt D.2-year review of a novel vestibular rehabilitation program in Montreal an Laval, Quebec. J Otolaryngol.2004, 33(1):5-9.
12. White J, Savvides p, Cherian N, Oas J. Canalith Repositioning for Benign Paroxysmal Positional Vertigo. Otology & Neurology. 2005, 26:704-10.
13. Nishino LK, Ganança CF, Manso A, Campos CAH, Korn GP. Reabilitação vestibular personalizada: levantamento de prontuários dos pacientes atendidos no ambulatório de otoneurologia da I.S.C.M.S.P. Rev. Bras. Otorrinolaringol. [periódico na Internet]. 2005 Ago [citado 2007 Fev 22]; 71(4): 440-447. Disponível em: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0034-72992005000400007&lng=pt&nrm=iso. doi: 10.1590/S0034-72992005000400007
14. Amá LAG, Amaral MC, Oliveira GC. Reabilitação Vestibular-Nossa Experiência. Rev Bras Otorrinolaringol. 1994, 60(2):113-16.
15. Yardley L, Masson E, Verschuur C, Haacket N, Luxon L. Symptoms, Anxiety and Handicap in dizzy patients development of vertigo symptom scale. J Psychosom Res. 1992, (36)8:731-41.
1. Master's Degree in Health Sciences at the Medical Sciences College of Santa Casa de São Paulo Phonoaudiologist responsible for the Otoneurology Service of the Otorhinolaryngology Department of ISCMSP.
2. Doctoral Degree in Otorhinolaryngology at the Federal University of São Paulo Assistant Professor of the Otorhinolaryngology Department of the Medical Sciences College of Santa Casa de São Paulo.
Institution: Irmandade Santa Casa de Misericórdia de São Paulo. São Paulo / SP - Brazil
Mail address:
Rua Dr. Cesário Mota Junior, 112 4º andar
São Paulo / SP - Brazil - Zip code: 01227-900
Article received on December 15, 2008.
Approved on December 18, 2008.
|
|
 |
|
|
