 |
575 |
|
| Year: 2008 Vol. 12 Num. 4 - Out/Dez - (16º)
|
|
 |
|
|
| Rhino-orbitocerebral Mucormycosis Associated with Cavernous Sinus Thrombosis: Case Report |
|
| Author(s): |
| Daniel Martiniano Haber1, Atílio Maximino Fernandes2, Dalisio De Santi Neto3, Renata Rennó Schiavetto4
|
|
|
| Key words: |
| mucormycosis, sinus thrombosis, immunossupression |
|
|
 |
| Abstract: |
Introduction: Mucormycosis is a rare opportunistic infection caused by Mucorales fungi, and the Rhizopus is the most common one (70% of the cases). It is an acute invasive fungal disease whose form is disseminated, cutaneous, pulmonary, gastrointestinal and rhino-orbitocerebral. The latter is the most common form and its symptoms comprise of unilateral sinusitis, fever and headache. Once established in the orbit the symptoms can be chemosis, diplopia and reduced vision. The infection can spread to the brain via the orbital apex, orbital arteries or via the cribriform plate. Mucormycosis is a medical emergency and the treatment consists of a surgery to an aggressive debridement and in the use of antifungal therapy. Despite the appropriate management, the mortality rate can reach 40% of the cases. One possible intracranial complication of Mucormycosis is the Cavernous Sinus Thrombosis which is a rare and fatal infective disease. The initial symptoms of Cavernous Sinus Thrombosis are headache, retro-orbital pain, periorbital edema, proptosis, diplopia and reduced vision. Case Report: We describe the case of 43-year-old woman with medical history of diabetes mellitus and use of immunosuppressant drugs after kidney transplantation. The patient developed Acute Bacterial Sinusitis and Rhino-orbitocerebral Mucormycosis associated with Cavernous Sinus Thrombosis.
|
|
 |
INTRODUCTION
The first description of mucormycosis was made by Paultauf in 1885 (1). This is a necrotizing disease caused by fungi of the Zygomycetes class and Mucorales order. From these, the most common genders found are Rhizopus (about 70% of the cases), Absidia, Mucor, Rhizomucor, Apophysomyces, Saksenaea, Cunninghamella, Cokeromyces and Syncephalastrum (2). These agents are commonly isolated from the ground and from decomposing animal and vegetal tissues. They can live in saprofitic association with normal individuals, and their cultivation is normal in upper airways material, mouth and feces of healthy people (2,3). The main route of infection is inhalatory. However, there may be traumatic transmission in polytraumatized patients, mainly with the Apophysomyces elegans. There are no reports of person-to-person transmission (4).
The mucormycosis is a rare and opportunist disease that mostly occurs in individuals with committed immunity, such as in solid organs transplantation, leukemia, lymphoma, myeloma, diabetes mellitus, extensive burns, renal insufficiency, hepatic cirrhosis, antineoplasic chemotherapy, chronic use of corticoids or immunosuppressive therapy (5). The development of mucormycosis is rare in other immunosuppressive states such as in AIDS or in immunocompetent patients (6).
Before the 60's the mucormycosis was almost always fatal, and with the discovery of Amphotericin B and its wide use associated with surgical debridement, the mortality rate was reduced to approximately 40% (2). This potentially fatal evolution is due to a certain specific characteristic of these fungi, which is vascular tropism, that initially invades the arteries and causes thrombosis and ischemic injuries. Then there occurs veins and lymphatic nodes invasion (7).
The mucormycosis may appear in pulmonary, cutaneous, disseminated, gastrointestinal and rhino-orbito-cerebral forms, and the latter is the most common one (8). In the rhino-orbito-cerebral mucormycosis, the most common complaints are purulent or bloody rhinorrhea, mostly unilateral, with fever, headache and general discomfort. When there is orbitary involvement, the complaints are of blepharelosis, diplopia and visual accuracy decrease. In the physical exam, there may appear unilateral or bilateral rhinorrhea, proptosis, chemosis, periorbitary cellulitis, alteration of the intrinsic and extrinsic ocular motoricity and amaurosis. The nasofibrolaryngoscopy may show necrotic lesions in the nasal mucosa (3,5).
The infection may be disseminated to the Central Nervous System through the orbitary apex, the cribriform plate or cause thrombosis in arteries that irrigate the Central Nervous System. The CNS is characterized by a change in the conscience level, convulsion and/or hemiplegia and with a worse prognostic (9).
A potential intracranial complication of mucormycosis is the Cavernous Sinus Thrombosis (CST). The first description of this affection was made by Duncan in 1821 (10). It's a rare infection that may appear from bacterial (more common) and/or fungal etiology. When caused by bacteria, it presented 80% of mortality and 75% of morbidity in the pre-antibiotic era and 13% and 23%, respectively, currently (11). In the Mucromycosis and CST the diagnosis must be early with aggressive therapy.
We reported a case of a patient who developed Acute Bacterial Rhinosinusitis and Rhino-orbito-cerebral Mucormycosis associated with CST.
CASE REPORT
The patient, female, 43 years of age, Black, sought, 10 months ago, the Otorhinolaryngology and Head and Neck Surgery Service of the Base Hospital of São José do Rio Preto, complaining of purulent rhinorrhea through the left nostril, headache, general discomfort and fever (not verified) for 7 years. She reported that one day before she began to have progressive and painful periorbitary edema in the left eye, retro-orbital pain to the left, diplopia and decrease of the visual accuracy in this eye. The patient reported a history of Systemic Arterial Hypertension (SAH) and Chronic Glomerulonephritis with Renal Transplantation 2 years ago. After this surgery, the patient developed a case of diabetes mellitus and used oral hypoglycemic agents (Metformin and Glibenclamide) and immunosuppressive agents (Prednisone 10mg/day, Tacrolimus 2mg every 12h and Mofetil Micofenolate-MMF 500mg every 12h). In addition to these medications, she also used antihypertensives (Captopril and Atenolol).
Upon physical exam the patient was conscious, oriented, in regular overall state, afebrile, tachicardic (FC=107bpm), with blood pressure of 130 x 75 mmHg and eupneic (FR=21ipm). The prior rhinoscopy showed hyaline secretion in the right nostril and purulent secretion (without fetid odor) through the left nostril. The ocular exam confirmed periorbitary edema with heat and hyperemia in the left eye, chemosis, proptosis, visual accuracy decrease, palpebral ptosis, ophthamoplegia and fixed mydriatic pupil in this eye. The nasofibrolaryngoscopy revealed purulent secretion in the left nasal cavity and necrosis area located in the left middle infundibulum head. The laboratory exams revealed leucocytosis with 13.300 leucocytes (VN=11.000) with prevalence of segmented elements (86%), blood sugar of 167 mg/dl and creatinine of 0.9 mg/dl (VN=0.6 to 1.0). 2 hemocultures were also requested, whose result was negative.
Faced with this case, we made the diagnostic hypothesis of Acute Bacterial Rhinosinusitis and Acute Invasive Fungal Rhinosinusitis associated with the Cavernous Sinus Thrombosis to the left and the patient was interned with Ceftriaxone 3g/day, Anfotericin B with initial dosage of 0.5mg/Kg/day, Intravenous Heparin 5000UI every 4 hours and the immunosuppressive drugs dosage was changed by the Renal Transplantation Service.
Computerized Tomography was requested for Face Sinuses and ophthalmologic evaluation. The CT revealed inflammatory sinusopaty with concealing of the maxillary sinus, ethmoidal cells and esphenoidal sinus in the left nasal cavity (Pictures 1 and 2). The exam didn't reveal changes to the extrinsic muscles or the left optical nerve. The ophthalmologic evaluation made the diagnostic hypothesis of retina central artery thrombosis with amaurosis in the left eye. The patient was also submitted to Nuclear Magnetic Resonance with angiographic study that showed indirect signs of Cavernous Sinus Thrombosis with thickening and enhancement of the contrast on the lateral wall of the left cavernous sinus (Pictures 3 and 4).
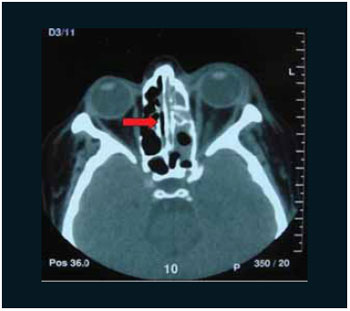 Picture 1. Computerized Tomography in axial cutoff with an arrow indicating the concealing of the front and rear ethmoidal cells and of the left esphenoidal sinus. 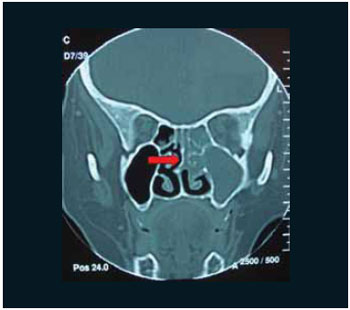 Picture 2. Computerized Tomography in coronal cutoff with an arrow indicating the concealing of the front and rear ethmoidal cells and of the left maxillary sinus.  Picture 3. Nuclear Magnetic Resonance in coronal cutoff with the arrow showing the thickening and enhancement of the left cavernous sinus lateral wall contrast. 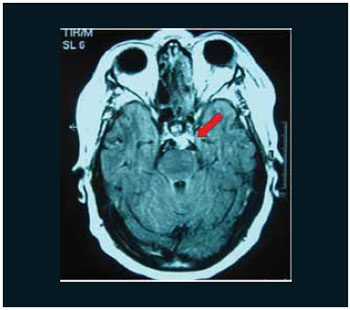 Picture 4. Nuclear Magnetic Resonance in axial cutoff with the arrow showing the thickening and enhancement of the left cavernous sinus lateral wall contrast.
In the 1st day of internment, the patient was also led to the surgical center and submitted to nasal endoscopic surgery with removal of necrotic areas of the left middle infundibulum, middle meatotomy and maxillary sinus Caldwell-Luc, ethmoidectomy and left esphenoidectomy. The necrotic material was sent for pathological evaluation and the left maxillary sinus secretion was sent for culture.
In the 1st post-operative period, the patient had an improvement of the overall state, but the complaints and the ocular exam remained unchanged. The nasofibroscopy revealed a moderate quantity of purulent secretion and the absence of necrosis areas in the left nasal cavity.
In the 2nd post-operative period the anatomopathologic evaluation revealed mucormycosis with extensive necrosis in the left middle infundibulum (Pictures 5 and 6) and in the maxillary sinus secretion culture there was a growth of Staphylococcus auerus. Therefore the Renal Transplantation service was discussed and we opted for the suspension of the Ceftriaxone and the introduction of Vancomycin. The medications dosage was daily adjusted according to the renal function (creatinine and creatinine clearance). The patient used Vancomycin for 21 days and Amphotericine B during 28 days, with a total antifungal dosage of 1.215g.
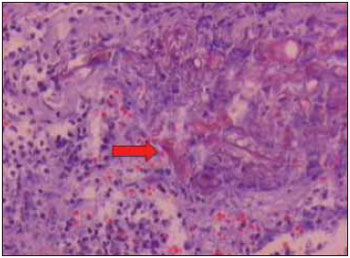 Picture 5. Arrow indicating fungal hyphas (Mucormycosis) agglomerated in the nasal mucosa necrotic area (HE - 200x). 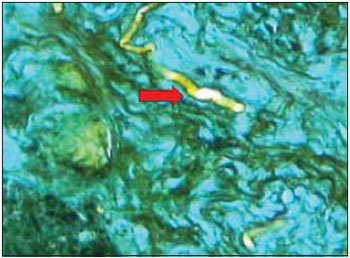 Picture 6. Arrow indicanting a fungal hyphas evident in the special preparation impregnated by silver (Grocott -200x).
During all the 31 days of internment, the patient was daily evaluated with nasofibroscopy and we didn't observe any new areas of necrosis in the nasal cavities. Even so, the patient remained with amaurosis, ophthalmoplegia and palpebral ptosis in the left eye. On the 31st day of internment, the patient received hospital discharge, and currently she receives follow-up from our service without evidence of the disease recurrence.
DISCUSSION
The Mucormycosis is a more fatal acute fungal infection for mankind, with mortality rate from 15 to 34% (12). The rhino-orbito-cerebral form is the most common form of Mucormycosis and occurs predominantly in patients with badly-controlled diabetes mellitus. Other populations that have a major risk to develop the disease are the patients with immunosuppression after organ transplantation, patients with malign hematological diseases, extensive burns, chronic use of corticosteroids or chronic renal insufficiency (5). In this case, the patient had as risk factors the diabetes mellitus, the chronic use of corticosteroids and immunosuppressive agents. The presence of Mucormycosis in the absence of the abovementioned factors is not very common (6).
The mucormycosis rhino-orbito-cerebral form is clinically confirmed with low fever, unilateral or bilateral rhinorrhea, unilateral facial pain, change in the visual accuracy and in the ocular movements as in the case reported (2, 3, 5). When present in the nasal cavity or in the paranasal sinuses, the mucormycosis may be spread to the orbit through the nasolacrimal duct, natural dehiscences in the papyraceous blade or through arteries and veins holes in the orbitary wall. The orbitary vases length may produce chemosis and proptosis (9). The fungal invasion may commit the ocular globe and the retina artery and produce amaurosis (2).
The initial complaints of the Cavernous Sinus Thrombosis are of retro-orbital pain, periorbital edema, chemosis, proptosis, palpebral ptosis and diplopia. Such symptoms are not specific and may be present in other affections as in the orbitary cellulitis. However, the presence of sepsis, paralysis of cranial pairs and bilateral ocular involvement are important signs for the CST. The CST diagnosis is made with the association of clinical signs and radiologic statements through the Computerized Tomography and/or the Nuclear Magnetic Resonance, and the latter is more sensitive to the diagnosis. This exam may reveal direct signs of CST such as changes to the signal intensity, the size and contour of the cavernous sinus and indirect signs like the thickening and enhancement of the contrast on the lateral wall of the cavernous sinus (14), as may be observed in the case reported. The CST occurs mostly due to the infections in the paranasal sinuses, mainly the ethmoid and the sphenoid ones (15). The agent that most commonly causes the CST is the Staphylococcus aureus, but this affection may also be caused by other bacteria or fungi (11). The early visual loss favors the suspicion of the retina artery commitment by Mucormycosis, but the amaurosis caused by the CST occurs more lately (3,7).
The case reported treats a patient with renal transplantation, bearer of diabetes mellitus, who chronically used corticosteroids and immunosuppressive agents and developed a case of Acute Bacterial Rhinosinusitis and Acute Invasive Fungal Rhinosinusitis (Mucormycosis) associated to the Cavernous Sinus Thrombosis. In this case it's not possible to define whether the CST was from bacterial, as in most cases, or fungal etiology (11). The patient was treated clinically with systemic antifungal agents (Amphotericin B), intravenous antibiotics (initially Ceftriaxone and after with Vancomycin) and with heparinization and with intranasal and Cadwell-Luc surgery with debridement of the nasal mucosa necrosis areas. The patient evolved with amaurosis and ophthalmoplegia in the left eye and is followed-up without new intercurrences.
CONCLUSION
The nasosinusal symptoms must always be evaluated in the immunosuppressed patients, as in the cases of organ transplantation, due to the major severity of the diseases in this group of individuals.
In the suspicion of Acute Invasive Fungal Rhinosinusitis (Mucormycosis), the treatment must be carried out quickly and aggressively, through the surgery for removal of the nasal mucosa necrosis areas and the use of intravenous systemic antifungal agents. Even so, there is a high rate of mortality and morbidity.
BIBLIOGRAPHICAL REFERENCES
1. Paulltauf A. Mycosis mucorina. Virchows Arch [A]. 1885, 102-543.
2. Yohai RA, Bullock JD, Aziz AA, Markert RJ. Survival factors in rhino-orbital-cerebral mucormycosis. Surv Ophthalmol. 1994, 39(1):3-22.
3. Bray WH, Giangiacomo J, Ide CH. Orbital apex syndrome. Surv Ophthalmol. 1987, 32(2):136-40.
4. Garcia-Covarrubias, L., R. Bartlett, D. M. Barratt, and R. J. Wassermann. Rhino-orbitocerebral mucormycosis attributable to Apophysomyces elegans in an immunocompetent individual: case report and review of the literature. J. Trauma. 2001, 50:353-7.
5. Pereira VG, Pereira MAA, Cruz JOB, Haron ES. Mucormicose rino-orbitária: Relato de um caso. Rev Hosp Clin Fac Med S. Paulo. 1982, 37(3):140-6.
6. Cuadrado LM, Guerrero A, Lopez Garcia Asenjo JA, et al. Cerebral mucormycosis in two cases of acquired immunodeficiency syndrome. Arch Neurol. 1988, 45:109.
7. Van Johnson E, Kline LB, Julian BA. Bilateral cavernous sinus thrombosis due to mucormycosis. ArchOphthalmol. 1988, 106(8):1089-92.
8. Prabhu RM, Patel R. Mucormycosis and entomophthoramycosis: a review of the clinical manifestations, diagnosis and treatment. Clin Microbiol Infect. 2004, 10 (suppl 1):31.
9. Ferry AP. Cerebral mucormycosis (phycomycosis). Ocular findings and review of the literature. Surv Ophthalmol. 1961, 6:1.
10. Duncan A. Contributions to morbid anatomy. Edinburgh Med Surg J. 1821, 17:321-36.
11. Yarington CT. Cavernous sinus thrombosis revisited. Proc R Soc Med. 1977, 70:456-9.
12. Fairley C, Sullivan TJ, Bartley P, et al. Survival after rhino-orbitalcerebral mucormycosis in an immunocompetent patient. Ophthalmology. 2000, 107:555.
13. Keane JR. Cavernous sinus syndrome. Analysis of 151 cases. Arch Neuro. 1996, 53:967-71.
14. Schuknecht B, Simmen D, Yuksel C, et al. Tributary venosinus occlusion and septic cavernous sinus thrombosis: CT and MR findings. Am J Neuroradiol. 1998, 19:617-26.
15. Stam J. Thrombosis of the cerebral veins and sinuses. N Engl J Med. 2005, 352:1791-8.
1. Otorhinolaryngologist. Otorhinolaryngologist for Hospital São Joaquim - UNIMED of Franca and Santa Casa de Franca - SP.
2. Otorhinolaryngologist Medical Doctor. Responsible for the Service of Rhinology of the Otorhinolaryngology and Head and Neck Surgery Department of the Base Hospital / FAMERP.
3. Pathologist of the Pathological Anatomy Service of the Base Hospital / FAMERP.
4. Resident Doctor in the 3rd year of the Otorhinolaryngology and Head and Neck Surgery Department of the Base Hospital / FAMERP.
Institution: Otorhinolaryngology and Head and Neck Surgery Department of the Base Hospital / College of Medicine of São José do Rio Preto - FAMERP. Franca / SP - Brazil.
Mail address:
Daniel Martiniano Haber
Rua Antônio Torres Penedo, 421, Sala 4 - Bairro São Joaquim
Franca / SP - Brazil - Zip code: 14406-352
Phone: (+55 16) 3701-3010 or Fax: (+55 16) 3711-7777
E-mail: danihaber@uol.com.br or danielhaber@bol.com.br
Article received on September 30, 2007.
Approved on May 21, 2008.
|
|
 |
|
|
