 |
628 |
|
| Year: 2009 Vol. 13 Num. 3 - Jul/Set - (7º)
|
|
 |
| Section:
Original Article
|
|
|
|
|
| Effectiveness of a Program of Auditory Prothetization in Elders Through the Application of HHIE-S Questionnaire |
|
| Author(s): |
| Roberto Dihl Angeli1, Geraldo Pereira Jotz2, Marion Cristine de Barba3, Pedro Guilherme Moeller Demeneghi4, Carolina Homrich Pereira de Mello5.
|
|
|
| Key words: |
| presbyacusis, elder's health, hearing loss, hearing impaired rehabilitation. |
|
|
 |
| Abstract: |
Introduction: The elders' hearing loss has been studied not only by the biological context, but also by the negative impact on the life quality of this population. The auditory prothetization is a basic part in the auditory rehabilitation. Objective: To evaluate the subjective impact of an auditory rehabilitation program in elders through the application of the HHIE-S questionnaire before and 30 days after rehabilitating therapy.
Method: 47 elder individuals were evaluated and 25 were male. The HHIE-S questionnaire was applied before and 30 days after auditory rehabilitation therapy. Result: The mean age of the sample was 75 years of age. 57% of the sample presented moderate hearing loss. The average score obtained passed from 24.2 to 1.8 points after the phonoaudiologic therapy period (p<0.001). Conclusion: The average scores were significantly reduced after 30 days of auditory prothetization and phonoaudiologic therapy. However, such results may be overestimated. The evaluation in 6 or 12 months may more faithfully measure the impact of a rehabilitating program in the elder's population life quality subjective perception.
|
|
 |
INTRODUCTION
The high prevalence of hearing loss in the elderly population, estimated between 36 and 45% (1-3), is not only a consequence of presbycusis, a degenerative process that results exclusively from aging (4), but also from the cumulative incidence of noise induced hearing loss (NIHL), sequels of otitis media and ototoxicity among other reasons. As a result, we identify in this population both sensorial and neurological auditory affection, which occurs separately or concomitantly.
In the last years, the hearing loss in the elderly has been approached not only by the strictly biological perspective, but also by its individual and collective impacts, taking into account, among others, the social, familiar and economic aspects.
Some studies have been showing the relationship between hearing loss and the commitment of quality of life of the elderly population (5, 6). There is a reduction of the verbal communication capacity, that leads to a progressive isolation and potentializes the appearing of depressive pictures. Likewise, there is a fall in the professional development irrespectively of the decline of physical or intellectual capacity, with economic echoes that may be remarkable, considering the high prevalence of families that are currently sustained by their elder members.
This recent importance of the concept of quality of life is reflected on the spread of questionnaires that aim to translate in an objective manner the discomfort or impact caused by the hearing losses, besides evaluating the effectiveness of the preventive and therapeutic measures. Amongst which, we may stand out APHAB (Abbreviated Profile of Hearing Aid Benefit), SHAPIE (Shortened Hearing Aid Performance Inventory for the Elderly) and SADL (Satisfaction with Amplification in Daily Life).
The HHIE questionnaire (Hearing Handicap Inventory for Elderly) has been widely used as a method for gauging the impact of hearing loss in elderly (6-8) Proposed by VENTRY and WEINSTEIN, in 1982 (9), it is originally composed by 25 questions that comprise individual, social and family aspects and its abbreviated version (Shortened, that originates the acronym HHIE-S) is composed by 10 questions.
The auditory prothetization duly indicated by the otorhinolaryngologist and followed up by therapy and phonoaudiologic rehabilitation is taken as an indispensible tool for the management of elderly with hearing loss (7,8). Therefore, this study aims to evaluate the effectiveness of a program of auditory prothetization in an elderly population through the application of the HHIE-S questionnaire before and after 30 days from the beginning hearing aid use and phonoaudiologic therapy.
METHOD
The project was approved by the Ethics Committee in Research of this University, under the number 2008105H.
The sample was composed by a retrospective cohort of 47 individuals, extracted at random from a population of 409 patients with equal age or older than 65 years attended in the High Complexity in Auditory Health department of the Otorhinolaryngology Service and Head and Neck Surgery of the Medical School of our University, during the period from January 16 2006 through January 31 2007.
The sample was computed as from the level of significance of 0.05, statistical power of 90% and a difference between population of 0.5 SD, which needed 44 individuals (or 88 verifications).
The attendance of the patients included in the Auditory Health Program meets the norm determined by Administrative Rule no. 587, of October 07 2004, of the Ministry of Health. The previous selection of the patents scheduled in this Program is made by professionals bound to the Public Health Service of the State, through the State Secretary of Health.
The patients are initially evaluated by an otorhinolaryngologist and submitted to audiological testing through imitanciometry and tonal and vocal audiometry exams. According to these results - and in case of medical indication - the patients are forwarded for performance of subsidiary exams, with register of encephalic trunk evoked potentials, for instance, or imaging exams.
The patients with clinical indication of auditory prothetization are guided in the phonoaudiological service for selection and fitting process. Under Administrative Rule no. 589, of October 8 2004, the adult patients must attend 4 sessions of rehabilitation (phonoaudiological therapy), within a period of 30 days. The sessions are individual and take 45 minutes. The professional who carries out the first therapy session is in charge of the subsequent sessions.
The rehabilitation is based on language and orofacial reading, in Ling sounds test and in the training of auditory abilities.
The HHIE-S questionnaire is applied by the phonoaudiologists of the Service before and after the rehabilitation period. Each of the 10 questions provides 3 answers: for each YES answer, 4 points are added; for each SOMETIMES answer, 2 points are added; for each NO answer, no point is added. The score obtained varies from 0 to 40 points.
For analysis of the hearing loss intensity, we used the average of tonal thresholds in 500, 1000 and 2000 Hz, as described by DAVIS and SILVERMAN, in 1970 (10).
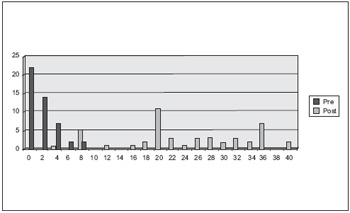 Figure 1. Distribution of the hearing loss intensity in the study's sample (n=47 patients).
RESULTS
The 47 patients who compose the studied sample had a mean age of 75 years and 4 months old (66 to 91 years), and 53% of the male sex. No patient had any picture secondary to chronic inflammatory process, although this had not been an exclusion previous criterion.
The auditory thresholds analysis confirmed that 27 patients (57%) had bilateral moderate hearing loss, 8 patients (17%) had bilateral light loss and only 1 patient had bilateral severe loss. The 11 remaining patients had asymmetric losses (Figure 1).
The average score obtained in the questionnaire before prothetization was of 24.2 points. The score obtained after 30 days was of 1.78 point. The difference between scores, measured through Student's t-test for independent samples, was statistically significant (p<0.001).
In the sample, 16 individuals (34%) had an equal or higher score than 30 points initially. Out of these, 5 had a score of 0 point after therapy. The total number of individuals who obtained 0 point after the therapy period was of 22, corresponding to 47% of the sample. The absolute frequency of the scores is shown in Figure 2.
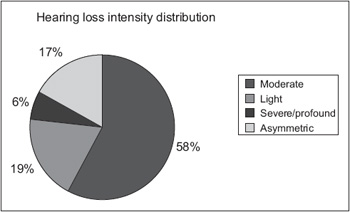 Figure 2. Distribution of HHIE-S score before and after rehabilitation therapy.
DISCUSSION
The hearing losses had effects on the quality of life that depend on characteristics of the loss (intensity, unilaterality, bilaterality, tinnitus, concomitant vertigo or otorrhea, time and speed of installation), the individual (sex, age, professional occupation, socioeconomic level, religiosity, education presence of concomitant diseases), family, social circle and even the community where the patient is inserted.
Therefore, the analysis of the tonal thresholds can evaluate only partially the impact of the individual quality of life loss.
The significant difference between the scores obtained before and 30 days after phonoaudiological therapy shows unequivocally the effectiveness of a multidisciplinary program of auditory rehabilitation for the elderly population.
The HHIE-S has been studied as a tracking tool in the elderly population (11-13). A few studies apply it to the analysis of medium or long terms benefits of a program of auditory rehabilitation.
Vuorialho and collaborators evaluated an auditory rehabilitation program of 98 elderly, and the average of the scores obtained by the HHIE-S was of 28.7 points. 6 months later, the average score fell to 12.7 points (7). In a Brazilian study that evaluated the HHIE-S scores of 7 individuals submitted to rehabilitation therapy, the average values, after 7 sessions, varied from 25.3 to 10.3 (8).
The average values obtained in our sample before the intervention were equivalent to those obtained in other works. Meanwhile, the average values after rehabilitation therapy were unequivocally low (Figure 3). For a better analysis of the real impact, we consider the questionnaire application to be more suitable after a longer period of time, ideally equal or longer than 6 months, since the tendency of the clinical therapeutics may be the overestimation of the initial impact (14, 15).
The low average of scores obtained 30 days after prothetization may also be justified by the general satisfaction of the patient with the service received by the multidisciplinary team, no matter the benefit caused separately by the intervention being studied.
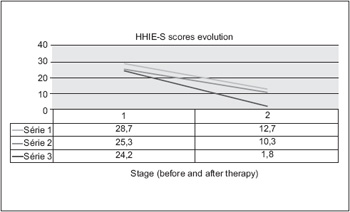 Figure 3. Evolution of the HHIE-S scores in this study (series 3) and comparison of the scores obtained in other studies (series 1 and 2).
CONCLUSION
The application of the HHIE-S questionnaire before and after the auditory rehabilitation therapy is an important tool for analysis of the impact on the quality of life both individually and collectively, but the outcomes may, equivocally, quantify this impact in an unreal manner. We believe the results after 6 or 12 months after auditory rehabilitation faithfully reflect the benefit the multidisciplinary follow up may provide the elderly population with.
BIBLIOGRAPHICAL REFERENCES
1. Béria JU, Raymann BCW, Gigante LP, Figueiredo AL, Jotz GP, Roithmann R, Costa SS, Garcez VR, Scherer CR. Hearing impairment and socio-economic factors: a population-based survey in an urban centre in southern Brazil. Rev Pan Salud Pub. 2007, 21(6):381-7.
2. Cruickshanks KJ, Wiley TL, Tweed TS, Klein BE, Klein R, Mares-Perlman JA, Nondahl DM. Prevalence of hearing loss
Angeli RD in older adults in Beaver Dam, Wisconsin. The Epidemiology of Hearing Loss Study. Am J Epidemiol. 1998, 148(9):879-86.
3. Sindhusake D, Mitchell P, Smith W, Golding M, Newall P, Hartley D, Rubin G. Validation of self-reported hearing loss. The Blue Montains hearing study. Int J Epidemiol. 2001, 30(6):1371-8.
4. Gates GA, Mills JH. Presbycusis. Lancet. 2005, 366(9491):1111-20.
5. Weinstein BE, Ventry IM. Hearing impairment and social isolation in the elderly. J Speech Hear Res. 1982, 25(4):593-9.
6. Dalton DS, Cruickshanks KJ, Klein BE, Klein R, Wiley TL, Nondahl DM. The impact of hearing loss on quality of life in older adults. Gerontologist. 2003, 43(5):661-8.
7. Vuorialho A, Karinen P, Sorri M. Effect of hearing aids on hearing disability and quality of life in the elderly. Int J Audiol. 2006, 45(7):400-5.
8. Marques ACO, Koslowski L, Marques JM. Reabilitação auditiva no idoso. Rev Bras Otorrinolaringol. 2004, 70(6):806-12.
9. Ventry IM, Weinstein BE. The hearing handicap inventory for the elderly: a new tool. Ear Hear. 1982, 3(3):128-34.
10. Davis H, Silverman SR. Auditory Test Hearing Aids. In: Davis H, Silverman SR. Hearing and Deafness. Holt, Rinehart and Winston, 1970.
11. Nondahl DM , Cruickhanks KJ, Wiley TL, Tweed TS, Klein R, Klein BE. Accuracy of self-reported hearing loss. Audiology. 1998, 37(5):295-301.
12. Lichtenstein MJ, Bess FH, Logan SA. Validation of screening tools for identifying hearing-impaired elderly in primary care. JAMA. 1988, 259(19):2875-8.
13. Gates GA, Murphy M, Rees TS, Fraher A. Screening for handicapping hearing loss in the elderly . J Fam Pract. 2003, 52(1):56-62.
14. Humes LE, Wilson DL, Barlow NN, Garner C. Changes in hearing-aid benefit following 1 or 2 years of hearing-aid use by older adults. J Speech Lang Hear Res. 2002, 45(4):772-82.
15. Malinoff RL, Weinstein BE. Amplification and aural rehabilitation. Ear Hear. 1989, 10(6):354-56.
1. Master's Degree in Otorhinolaryngology at the Federal University of Rio Grande do Sul (UFRGS). Assistant Professor of the Medical Course of the Lutheran University of Brazil (ULBRA).
2. Post-Doctoral Degree in Otorhinolaryngology at the University of Pittsburg, USA. Assistant Professor of the Medical Course of the Lutheran University of Brazil (ULBRA).
3. Master's Degree in Communication Disorders at Universidade Tuiuti do Paraná. Phonoaudiologist of the High Complexity Program in Auditory Health of the Lutheran University of Brazil (ULBRA).
4. Specialist in Otorhinolaryngology at ABORL-CCF. Contracted Doctor in the Otorhinolaryngology Service and Head and Neck Surgery at the Lutheran University of Brazil (ULBRA).
5. Medical Course Student of the Lutheran University of Brazil (ULBRA). Researcher of the High Complexity Program of Auditory Health of the Lutheran University of Brazil (ULBRA).
Institution: Programa de Alta Complexidade em Saúde Auditiva - Serviço de Otorrinolaringologia e Cirurgia de Cabeça e Pescoço - Hospital Universitário -Universidade Luterana do Brasil (ULBRA). Porto Alegre / RS - Brazil. Mail Address: Roberto D. Angeli - Rua Plínio Brasil Milano, 80 - Bairro Auxiliadora - Porto Alegre / RS - Brazil - Zip code: 90520-900 - Telephone: (+55 51) 3337-3460 - E-mail: roberto.dihl@terra.com.br
Article received on July 6 2009. Approved on August 1 2009.
|
|
 |
|
|
