 |
652 |
|
| Year: 2009 Vol. 13 Num. 4 - Out/Dez - (9º)
|
|
 |
| Section:
Original Article
|
|
|
|
|
| Aspiration Biopsy by Fine Needle of Cervical Adenopathy Guided by Ultrasonography |
|
| Author(s): |
| Rogério Aparecido Dedivitis1, Elio Gilberto Pfuetzenreiter Jr.2, Mario Augusto Ferrari de Castro3.
|
|
|
| Key words: |
| lymph nodes, needle biopsy, intervention ultrasonography, lymphadenitis, lymphoproliferative disorders, lymphatic metastasis. |
|
|
 |
| Abstract: |
Introduction: The fine needle aspiration biopsy (FNAB) is deemed to be a diagnostic option replacing the lymph nodes open dissection. Nevertheless, the diagnosis obtained is frequently insufficient clinically. Objective: To evaluate the accuracy of FNAB diagnostic guided by ultrasonography (USG) in the cervical adenopathy approach. Methods: Consecutive series study of 186 patients who were submitted to retrospective USG-guided FNAB of cervical adenopathy. The final diagnosis was determined by the biopsy histopathological exam by excision of the lymph node when applied or clinical follow-up for more than one year. Sensitivity, specialty, predictive values and accuracy were evaluated. Results: There was a total of 54 malignancy diagnosis, five of tuberculosis and 127 of nonspecific chronic lymphadenitis. The sensitivity, specificity, predictive values of the negative and positive tests and FNAB accuracy were respectively of 79.5%, 99.1%, 88.2%, 98.3% and 91.4%. Conclusion: As the positive FNAB is highly predictive of the final histological diagnosis, the negative result must be carefully interpreted.
|
|
 |
INTRODUCTION
The cervical adenopathy may appear as a consequence of a benignant or malignant disease. The fine needle aspiration biopsy (FNA) is largely used for its evaluation, however, it presents some limitations due to inconclusive samples and the high rate of false-negative (1). When the FNAB is applied for the cervical adenopathy study to clarify and results in non-diagnostic, there may be the need for open biopsy. However, the excisional or incisional biopsy of a lymph node require hospital admission, may be sometimes of general anesthesia and is susceptible to complications (2).
One of the differential diagnoses are the lymphomas. In the past, the standard procedure for its diagnosis was the excisional biopsy, and, today, about two thirds of the cases are detected by FNA; but it is essential to determine the nodal architecture and to have sufficient samples to carry out the immunophenotyping, in which the method finds limitation (3).
The incorporation of the imaging methods upon performance of biopsies has improved the possibilities of research, specially when the lymph nodes to be evaluated are in a deeper location, and avoids, in many cases, the open surgery as a first diagnostic procedure (4). Due to its accuracy, non-invasivity and no need to expose the patient to radiation, the ultrasonography aiming at guiding the act of collection of material for the head and neck masses during FNAB is indicated before a surgical approach (5).
The objective of this study is to evaluate the diagnostic accuracy of FNAB guided by ultrasonography in the approach of the cervical adenopathy.
METHOD
A total of 186 patients previously treated was submitted to cervical adenopathy FNAB from February 1995 through February 2008. Record data and the cytopathologic findings were collected retrospectively. The patients' age ranged from 7 to 90 years, with mean age of 55 years. From the total, 130 patients were male, with male:female ratio of 2.32:1. All patients presented with cervical adenopathy symptom, with history time ranging from one to six months (mean time of three months). The inclusion criteria for performance of FNAB were: cervical adenopathy with duration longer than one month from unexplained cause and measuring, in the major lymph node axis, at least one centimeter of diameter. Platelet count and coagulation exams were not carried out on regular basis. The FNAB was performed by means of disposable syringe of 10mL and hypodermic needle of 20 x 5.5mm. All the biopsies were guided by ultrasonography in the mode B, with a 10mHz resolution set. The Papanicolaou stain was applied. The biopsy procedure was repeated when, according to visual criterion, the sample collected was inadequate, specially when it came hemorrhagic.
The database was composed by demographic, clinical and pathological data. The cytopathologic findings were divided into inconclusive (insufficient material for analysis), benign (unspecific lymphadenitis), suspicion of granulomatous and malignancy disease. Sensitivity, specificity, predictive values for positive and negative tests and accuracy were computed, having as gold standard, when proceeded, the specimen histopathological result included in paraffin or, then, we carried out clinical follow up (and if required, ultrasonographic complementation) of the other patients for at least one year. The FNAB findings were classified as true-negative (absence of correctly diagnosed malignancy), true-positive (presence of correctly diagnosed malignancy), false-negative (failure of the method to diagnose malignancy) and false-positive (material incorrectly considered to be malignant or suspect of malignancy).
RESULTS
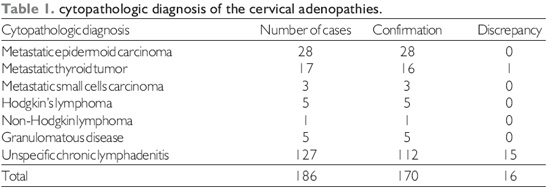
A total of 186 patients was included in this study. Table 1 shows the distribution of the cases according to the cytopathologic result and its correlation to the ultimate findings, based on the histopathological findings or, in the cases of unspecific chronic lymphadenitis, from a follow up of at least one year without evidence of a more aggressive etiology. Out of the 127 cases compatible with lymphadenitis, 29 were paucicellular or with hemorrhagic material; however, do to the lymphoid population they were not interpreted as inconclusive.
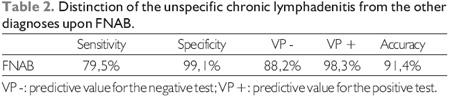
Table 2 shows the FNAB accuracy, which presented sensitivity of 79.5%, specificity of 99.1%, negative and positive tests predictive values of 88.2% and 98.3%, respectively, and accuracy of 91.4%.
All 28 patients whose biopsy revealed a trait of carcinoma had their diagnosis confirmed. Out of whom, nine had cervical metastasis with occult primary tumor; eight had lymph node recurrence after previous oncologic treatment; six had primary tumor diagnosed in a primary site in the upper aerodigestive tract with neck classified clinically as N0 and with a finding of adenopathy upon computed tomography; and five were occasional findings. In 17 cases, the diagnosis was of papilliferous carcinoma of metastatic thyroid. Out of these, in ten, the patient had already been previously treated and it was a late recurrence, while, in seven, the patients had not been treated and had no diagnosis of the gland primary disease. There were three cases with small cells carcinoma metastasis which fully confirmed pulmonary primary lesion upon research. As for the cases of confirmed by FNAB of lymphoma, out of the six, five included Hodgkin's disease, and it was possible to carry out the immunophenotyping in two cases without need for extirpation of the lymph node.
Out of 127 cases diagnosed as unspecific chronic lymphadenitis (reactional hyperplasia), 16 ended up with indication of biopsy for histopathological evaluation, with diagnosis of lymphoma in 11 and of tuberculosis in five. Out of these lymphomas, six comprised Hodgkin's disease and five comprised non-Hodgkin's lymphoma. As for the remaining 112 cases, 13 were submitted to biopsy, with confirmation of the biopsy impression - unspecific inflammatory process. The other 99 cases were clinically followed up for at least one year without change in their clinical pattern.
DISCUSSION
The image method guided FNAB has been becoming more and more popular in the diagnostic approach of cervical adenopathy. There is evidence that the diagnosis of lymph nodes deeply located may be led by minimally invasive procedures, as in the guided FNAB or even by video-guided surgery; however, there are authors who prioritize the open biopsy for superficial lymph nodes. Nevertheless, we must consider the guided FNAB as a tracking procedure for peripheral lymph nodes. (4).
The FNAB cytopathology exam is a safe and efficient procedure for the diagnosis of cervical adenopathy. But it has some limitations even when carried out under optimal condition. It may be difficult to tell low degree lymphoma from reactional hyperplasia and the lymphoma may not be definitive. The diagnostic suspicion generated may indicate the need for the lymph node excision for histological evaluation of the whole organ architecture shape (6). The lymph nodes FNAB also has a relatively high rate of inconclusive results that may sometimes be reported as "negative for malignancy" and be problematic for the adenopathy approach, since some benign diseases, such as ganglionar tuberculosis or scrofulosis, require the proceeding of a suitable treatment (1).
Insufficient material may cause discrepancies in 25% of all cases. It is grounded on necrosis, hemorrhage and presence of paucicellular material with artifacts that make the diagnosis difficult. This may be decreased by the presence of the pathologist in loco who may assure the obtainment of suitable material (7).
In patients with a lymph node single group suggesting lymphatic draining from a solid tumor or in patients with risk factors (use of alcohol and smoking, for instance), it is strongly recommended to search for the primary tumor before lymph node biopsy. This recommendation is particularly relevant in the cervical region, where the metastases derived from the upper aerodigestive tract mucosa are common.
In our study, the guide FNAB results by ultrasonography were precise in the establishment of metastatic disease. All 28 cases of carcinoma original from the upper aerodigestive tract, as well as 16 out of the 17 cases of metastasis of thyroid papilliferous carcinoma were correctly diagnosed. As for the cases of lymphoma there was no false-positive result, that is, they were six true-positive cases. On the other hand, out of the 127 cases whose FNAB was compatible with unspecific lymphadenitis, 11 were lymphomas and five were ganglionar tuberculosis. Additionally, only in two cases of lymphoma correctly diagnosed it was possible to proceed with an accurate subclassification.
Out of the benign causes of unexplained cervical adenopathy, the ganglionar tuberculosis is important, because the medication schema must be established as soon as possible. Therefore, the ready and accurate diagnosis is important, and it cannot always be obtained by means of imaging methods. The sensitivity and the accuracy are not very high in such cases, specially due to the inconclusive samples (8). In our sample, there were five true-positive for granulomatous disease and five false-negative, initially interpreted by the FNAB as reactional hyperplasia that, due to the clinical suspicion, ended up referred to for lymph node biopsy.
In spite the guided FNAB by imaging method may be carried out within one or two days, the open biopsy is not made as quickly. The surgical lymphadenectomy requires a surgeon, an assistant, a surgical room and all costs involved. In addition to this, it is not an innocuous procedure and is susceptible to complications, such as seroma, lymphoceles, pieces edge necrosis, wall infection, edema and thromboflebitis (9). Moreover, there may occur not much aesthetical scar and residual pain, sometimes in diseases whose treatment will not be surgical. Some complications may delay the beginning of chemotherapy, when it is indicated. Another advantage of the FNAB over excisional biopsy is that it allows the maintenance of the lymph node in its anatomic site, by enabling the monitoring of the therapeutic response and even proceeding with a future biopsy (4).
This study supports the performance of FNAB guided by ultrasonography, as it is a minimally invasive procedure and without significant complications; as well as, in many cases, it provides conclusive results that may guide the therapeutic procedures. Nevertheless, in stratified cases such as negative results, it is essential that the clinical suspicion be valuated and the open biopsy be indicated.
CONCLUSION
While the positive FNAB is highly predictive of the final histological diagnosis (predictive value for the positive test of 98.3%), the negative result must be interpreted as a precaution (predictive value for the negative test of 88.2%), with failures in the diagnoses of lymphoma and tuberculosis.
BIBLIOGRAPHICAL REFERENCES
1. Kim BM, Kim EK, Kim MJ, Yang WI, Park CS, Park SI. Sonographically guided core needle biopsy of cervical lymphadenopathy in patients without known malignancy. J Ultrasound Med. 2007, 26(5):585-91.
2. McGuirt WF, McCabe BF. Significance of node biopsy before definitive treatment of cervical metastatic carcinoma. Laryngoscope. 1978, 88(4):594-7.
3. Hehn ST, Grogan TM, Miller TP. Utility of fine-needle aspiration as a diagnostic technique in lymphoma. J Clin Oncol. 2004, 22(15):3046-52.
4. de Kerviler E, de Bazelaire C, Mounier N, Mathieu O, Brethon B, Brière J, Marolleau JP, Brice P, Gisselbrecht C, Frija J. Image-guided core-needle biopsy of peripheral lymph nodes allows the diagnosis of lymphomas. Eur Radiol. 2007, 17(3):843-9.
5. Welkoborsky HJ. Ultrasound usage in the head and neck surgeons office. Curr Opin Otolaryngol Head Neck Surg. 2009, 17(2):116-21.
6. Layfield LJ. Fine-needle aspiration of the head and neck. Pathology (Phila). 1996, 4(2):409-38.
7. Fathallah L, Tulunay OE, Feng J, Husain M, Jacobs JR, Al-Abbadi MA. Histopathologic and cytopathologic diagnostic discrepancies in head and neck region: pitfalls, causes, and preventive strategies. Otolaryngol Head Neck Surg. 2006, 134(2):302-8.
8. Ammari FF, Bani Hani AH, Ghariebeh KI. Tuberculosis of the lymph glands of the neck: a limited role for surgery. Otolaryngol Head Neck Surg. 2003, 128(4):576-80.
9. Picardi M, Gennarelli N, Ciancia R, De Renzo A, Gargiulo G, Ciancia G, Sparano L, Zeppa P, Martinelli V, Pettinato G, Lobello R, Pane F, Rotoli B. Randomized comparison of power Doppler ultrasound-directed excisional biopsy with standard excisional biopsy for the characterization of lymphadenopathies in patients with suspected lymphoma. J Clin Oncol. 2004, 22(18):3733-40.
1. Post-Doctoral Degree at the Fundação Lusíada UNILUS, Santos. Head Professor of Otorhinolaryngology and Head and Neck Surgery of the Metropolitan University of Santos.
2. Master's Degree in Sciences in the Post-Graduation Course of Hospital Heliópolis, São Paulo / SP. Professor of the Surgery Department of the Fundação Lusíada UNILUS, Santos. Assistant of the Head and Neck Surgery Services of the Hospital Ana Costa and of Irmandade Santa Casa de Misericórdia de Santos, Santos / SP, Brazil.
3. Resident Doctor of Head and Neck Surgery at Hospital Ana Costa, Santos. Professor of the Surgery Department of the Fundação Lusíada UNILUS, Santos / SP, Brazil.
Institution: Serviços de Cirurgia de Cabeça e Pescoço do Hospital Ana Costa e da Irmandade da Santa Casa da Misericórdia de Santos. Santos / SP - Brazil. Mail Address: Rogério A. Dedivitis - Rua Dr. Olinto Rodrigues Dantas, 343 - Conj. 92 - Santos / SP - Brazil - Zip code: 11050-220 - Telephone: (+55 13) 3223-5550 / 3221-1514 - E-mail: dedivitis.hns@uol.com.br. Article received on November 8 2009. Approved on November 30 2009.
|
|
 |
|
|
