 |
724 |
|
| Year: 2010 Vol. 14 Num. 4 - Out/Dez - (9º)
|
|
 |
| Section:
Original Article
|
|
|
|
|
| Efficacy of Endoscopic Sinus Surgery in the Treatment of Chronic Rhinosinusitis |
|
| Author(s): |
| Flávia Machado Alves Basílio1, Murilo Carlini Arantes2, Annelyse Cristine Ballin3, Moises Rafael Dallagnol2, Mathias Bohn Bornhausen4, Denilson Cavazzani Szkudlarek2, Marco César Jorge Santos5, Marcos Mocellin6.
|
|
|
| Key words: |
| Sinusitis, Symptoms, Treatment outcome. |
|
|
 |
| Abstract: |
Introduction: The endoscopic sinus surgery (FESS) is currently regarded as the gold standard in the treatment of chronic rhinosinusitis (RNSC), with or without nasal polyposis refractory to medical therapy optimized. Objective: To evaluate the improvement of symptoms after FESS RNSC, through a questionnaire. Method: This is a prospective study, which included 34 patients undergoing FESS during the year 2009, the Service of Otorhinolaryngology, Hospital das Clínicas / UFPR. Of these, 22 were diagnosed as RNSC RNSC and 12 had associated nasal polyps. All patients underwent a questionnaire on preoperative symptoms, comorbidities and degree of symptom improvement after surgery, six months after the procedure. Results: The percentage improvement of symptoms more prevalent in the group with RNSC was as follows: nasal obstruction 87.4%, 80.5% headache, pain / facial pressure 91.6% 81.2% posterior nasal discharge. In the group with polyposis associated improvement was nasal obstruction 76.6%, 76.6% posterior nasal discharge, hyposmia, 68.7%, headache 83%. In our study we found an overall improvement in symptoms of 83.74% in patients with RNSC and 80.5% in patients with associated nasal polyposis. Conclusion: FESS is highly effective in controlling symptoms of RNSC with or without polyposis and is, in our study, its efficacy similar to that found in the literature. With respect to patients with nasal polyposis, studies are needed with longer follow up, since this disease has a high degree of recurrence.
|
|
 |
INTRODUCTION
Functional endoscopic sinus surgery (FESS) is nowadays regarded as the gold standard for treatment of chronic rhinosinusitis (CRS), with or without nasal polyposis refractory to optimal medical treatment. This surgery is based on the principles of improved function and patency of the complex bone-meat (COM), through interventions in the sidewall of the nose (1).
The surgical technique was standardized and popularized by KENNEDY (2) in the early 80s, and since then, the indications for this procedure has increased due to its good results. A total success rate of 80% to 98% is reported in the literature, most often without an accompanying long-term (3-10). But even with good technique, the clinical course of disease can be challenging due to various factors involved in the pathophysiology of CRS.
In this study, we sought to evaluate the prevalence of various symptoms of CRS, with or without nasal polyps, and analyze the effect of endoscopic surgery on these symptoms through a questionnaire developed at our institution.
METHOD
This is a prospective study approved by the Ethics Committee on Human Research of Hospital de Clínicas / UFPR (CEP). The study addresses aspects of Resolution CNS 196/96, and others on Guidelines and Standards for Research involving human subjects of the Ministry of Health registry on ZIP: 2247.141/2010-06.
The study included 34 patients undergoing FESS during the year 2009. Of these, 22 diagnosed with CRS and 12 with CRS associated with nasal polyposis. All with clinical and radiological diagnosis of diseases and refractory to optimal medical treatment prior to surgical indication. We excluded patients with recurrent polyps and those who underwent re-operation.
The surgeries were performed at the Hospital de Clinicas, Federal University of Parana, under general anesthesia by residents of the third year under the supervision of the preceptor. The surgical procedure consisted of septoplasty and polypectomy, if necessary, and partial middle turbinectomy in all cases. As (s) breast (s) paranassal (s) effect (s), the surgical technique used was described by MESSERKLINGER (1) and STAMMBERGER (4). At surgery, nasal packing was used only in cases of persistent nosebleeds.
The system of internment was the day hospital, with follow-up after surgery in 2 days, 7 days, 30 days and 3 months and 6 months. Regarding postoperative treatment was used levofloxacin for 10 days, prednisone 20 mg / day for 5 days, paracetamol for pain, topical neomycin and nasal saline solution in both groups. In the postoperative follow-up were cleaning and removal of nasal crusts.
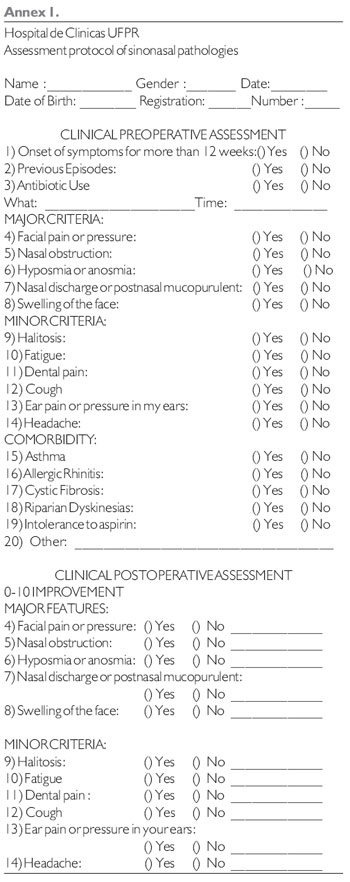
All patients underwent a questionnaire (Appendix 1) on the preoperative symptoms, comorbidity and degree of symptom improvement postoperatively. The evaluation of symptoms after surgery was performed six months after the procedure. Patients were asked to evaluate the improvement of each symptom ranging from 0 to 10, zero being the absence of improvement and ten to complete improvement of symptoms, compared to the state prior to surgery.
The patients signed a consent form approved by the ethics committee of the hospital and were duly informed about the study proposal, collaborating in that had their personal information kept private.
RESULTS
Among the 34 patients studied, 21 patients were female and 13 male. Twenty-two were diagnosed with CRS and 12 patients had a diagnosis of CRS associated with nasal polyposis. The mean age was 38.15 years in group CRS and 43.45 years in patients with nasal polyps. In both groups the improvement of all symptoms was higher than 60%.
With regard to comorbidities, in patients with CRS 9% (2) had asthma, 86.3% (19) allergic rhinitis, and none had ciliary dyskinesia or cystic fibrosis. In the group with nasal polyps found associated asthma in 16.6% (2), allergic rhinitis in 91.6% (11), and 1 patient with intolerance to aspirin, also had no patients with ciliary dyskinesia or cystic fibrosis in this group.
Table 1 lists the incidence of symptoms in both groups. In patients with CRS, the most prevalent symptoms were nasal obstruction (95.45%), headache (86.3%), facial pain / pressure (81.8%), posterior nasal discharge (77.2%) . In patients with nasal polyps, the symptoms were nasal obstruction (100%), posterior nasal secretion (100%), hyposmia (91.6%), headache (83.3%).Important differences regarding symptoms of both groups were observed: the presence of facial pain / pressure: 81.8% in the first group, against 58.3% in patients with nasal polyps; cough: 36.3% for the CRS versus 66 , 6% in patients with nasal polyposis.
Table 2 lists the percentage improvement after surgery, the symptoms reported. All symptoms showed improvement over 60%. In CRS group with the percentage of improvement was most prevalent symptoms: nasal obstruction 87.4%, 80.5% headache, facial pain / pressure 91.6% 81.2% posterior nasal secretion. In the group with polyps associated with improvement percentage of the prevalent symptoms were: nasal obstruction 76.6%, 76.6% posterior nasal secretion, hyposmia, 68.7%, headache 83%. Chart 1 illustrates these results, which reflect the effectiveness of endoscopic surgery.
DISCUSSION
Rhinosinusitis is characterized by inflammation of the nose and paranasal sinuses, thus becoming one of the most common disorders of the upper airways. Can be classified according to Brazilian Guidelines on Rhinosinusitis (12) in acute (lasting 4 weeks), subacute (duration between 4 and 12 weeks) and chronic (lasting longer than 12 weeks).
In relation to chronic rhinosinusitis (CRS), the target of our study, the estimated incidence of 15% of pathology at the U.S. population (3). Brazil still lacks statistics on prevalence and incidence related to CRS.
The diagnosis of these diseases is based on clinical criteria. The major symptoms of CRS are nasal congestion, facial pressure sensation, nasal obstruction, rhinorrhea and hyposmia, and minor symptoms: headache, toothache, halitosis, fatigue, dry cough, fever and pain. The presence of two major factors, a major factor and two minor or the presence of pus in the nasal cavity suggested the diagnosis of CRS. Tomography of the paranasal sinuses with changes resistant to medical treatment is also considered diagnostic (13). The symptoms described by patients guide the conduct of the physician, both in relation to treatment, as to the application of endoscopy and computed tomography scans, the main tools for diagnosing and evaluating the severity of CRS (14).
The outcome of FESS, similarly, can be evaluated by objective and subjective methods. In clinical practice, the welfare of the patient seems to be reliable in isolation, but the objective assessment can also be accomplished through additional tests. STAMMBERGER (4), in a study including 500 patients with subjective improvement rate of 91% found that the improvement in objective evaluations were below the status of well-being of the patient. In our study, we evaluated the profile of essentially subjective improvement through a visual analogue scale (VAS) using a questionnaire developed in our department, not validated in the literature.
Severity of Symptoms of Rhinosinusitis (EVA)
0__________________________________10
No symptoms Biggest hassle imaginable
The most prevalent symptoms in this study were: nasal obstruction, headache, facial pain, postnasal discharge and hyposmia, which is in agreement with the literature (4,7). Its effects were respectively: 95.45% 86.3% 81.8% 81.2% 72.7% in patients with CRS and polyposis in the group we find: 100%, 83%, 58.3% , 100% and 91.6%. Compared with the national study conducted in 2006 at the Hospital de Clinicas, Federal University of Pernambuco (8) gives 100% nasal obstruction, headache in 87.5%, 91.6% in rhinorrhea and hyposmia in 83.3%, the which shows correlation between the incidence of symptoms. In the same study, the improvement of nasal obstruction was 92.3% in patients with nasal polyps, 76.6% in our study. In the patients with CRS without polyps improvement was 72.7% against 87.4% of our patients. In relation to the headache, we found an improvement of 80.5% in the group without polyps and 83% in patients with polyposis. Respectively, the study of Pernambuco had rates of 54.5% and 70%.
When considering the overall success rates in the postoperative period, the results of FESS are very satisfactory. An improvement rate of 80% to 98% in this sense is found for FESS in the literature (3-10). The authors attribute this small percentage of failure to different factors in the pathophysiology of the disease, including environmental factors like pollution, dust and cigarette smoke (9). In the study by Damm (10) the overall improvement after surgery was 85%, while Bhattcharyya (7) described improvement in 100% of patients, especially in the following symptoms: facial pain, congestion, nasal obstruction, rhinorrhea, and headache. In a similar study conducted at University Hospital of Pernambuco (8) found an overall improvement in 50% of patients, 54.2% of cases reported considerable gain in quality of life. In the study by Dursun (11) and colleagues, which examined the predictors of success in CRS FEES, was hit success of FESS in 83% of cases, 54.4% had associated nasal polyposis. In our study, despite the shorter length of postoperative follow-up, we found a global improvement in symptoms of 83.74% in patients with CRS and 80.5% in patients with associated nasal polyposis, which showed similarity with the international literature and a percentage of greater improvement compared to the national study cited.
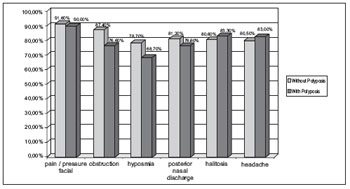 Graphic 1. Improves of symptoms percentage.
CONCLUSION
Functional endoscopic sinus surgery (FESS) is highly effective in controlling symptoms of CRS, either with or without nasal polyps. In our study we evaluated subjectively the overall clinical improvement and symptomatic after the procedure. Despite the shorter length of postoperative follow-up, the results were similar to those found in the literature. Also in relation to patients with nasal polyposis, more studies are needed, since this disease has a high degree of recurrence.
BIBLIOGRAPHIC REFERENCES
1. Messerklinger W, Endoscopy of the nose. Munich: Urban & Swarzenberg; 1978:49-50
2. Kennedy DW, Functional Endoscopy sinus surgery technique. ArchOtolaryngol. 1985, 111:643-49.
3. Kaliner MA, Osguthorpe JD et al. Sinusitis: bech to beside- current findings, future directions. J Alergy Clin Immunol. 1997, 99:S829-S48.
4. Stammberger H, Michael Hawke. Polipose nasal. Em: Cirurgia endoscópica dos seios paranasais. Ed. Revinter; 2002. p.96-105.
5. Levine HL. Functional endoscopic sinus surgery: evaluation surgery and follow up of 250 patients. Laryngoscope. 1990, 100:79-84.
6. Schaitkin B, May M, Shapiro A, et al. Endoscopic sinus surgery: 4-year follow-up on the first 100 patients. Laryngoscope. 1993, 103:1117-20.
7. Bhattacharyya N. Symptom Outcomes After Endoscopic Sinus Surgery for Chronic Rhinosinusitis. Arch Otolaryngol Head Neck Surg. 2004, 130:329-33.
8. Bunzen DL, Campos A, Leão FS, Morais A, Sperandio F, Caldas Neto S. Eficácia da cirurgia endoscópica nasal nos sintomas da rinossinusite crônica associada ou não à polipose. Rev Bras Otorrinolaringol. 2006, 72(2):242-246.
9. Danielsen A, Olofsson J. Endoscopic sinus surgery. A long-term follow-up study. Acta Otolaryngol (Stockh). 1996, 116:611-9.
10. Damm M, Quante G et al. Impact of functional Endoscopy Sinus Surgery on Symptoms and Quality of Life in Chronic Rhinosinusitis. Laryngoscope. 2002, 112:310-5.
11. Dursun E, Korkmaz H, Eryilmaz A. Clinical predictors of long-term success after endoscopic sinus surgery. Otolaryngol Head Neck Surg. 2003, 129(5):526-31.
12. Diretrizes Brasileiras de Rinossinusite. Rev Bras Otorrinolaringol. 2008, 74(2,supl):6-59.
13. Lanza DC, Kennedy DW. Adult rhinosinusitis defined. Otolaryngol Head Neck Surg. 1997, 117(3 pt 2):S1-S7.
14. Gliklih RE, Metson RB. A comparison of sinus computed tomography (CT) staging systems for outcomes research. Am J Rhino. 1994, 8:291-7.
1 Scholar. PhD.
2 Otorhinolaryngologist.
3 Third Year Resident of Otolaryngology UFPR.
4 Academic Sixth Year of Medical School UFPR.
5 Otorhinolaryngologist. Collaborating Medical Residence in Otorhinolaryngology, Hospital de Clinicas - UFPR.
6 Professor and Head of the Department of Otolaryngology, Hospital de Clinicas - UFPR.
Institution: Hospital de Clinicas, Federal University of Parana. Curitiba / PR - Brazil. Mail Adress: Basil Alves Flávia Machado - Rua Brigadeiro Franco, 2477 - Apto. 1202 - Centro - Curitiba / PR - Brazil - Zip code: 80250-030 - Telephone: (+55 41) 3222-3797 / (+55 41) 9191-5001 - E-mail: flavia_mab@yahoo.com.br
Article received on July 23, 2010. Approved on August 22, 2010.
|
|
 |
|
|
